TriageIQ Revolutionizing Healthcare with GenAI-Based Triage
Explore TriageIQ and its unique features in healthcare, delving into GenAI-based triage systems, their integration, decision support, specialized algorithms, and resource optimization in medical settings.


Generative Artificial Intelligence (GenAI) and broader AI technologies are poised to fundamentally reshape healthcare triage, offering transformative potential to address long-standing systemic inefficiencies. This report explores the conceptual framework of "TriageIQ," representing the intelligent application of AI to optimize patient assessment, prioritization, and resource allocation. AI's capacity to analyze vast datasets, predict clinical outcomes, and automate routine tasks promises enhanced decision-making, improved operational efficiency, and a more standardized approach to patient care. However, the successful integration of these technologies is not without its complexities. Critical challenges, including algorithmic bias, data privacy concerns, and the imperative of fostering human trust and effective human-AI collaboration, necessitate careful consideration and proactive mitigation strategies. Despite these hurdles, the trajectory of GenAI in healthcare triage points toward an era of hyper-personalized, proactive care, driven by multimodal AI models, synthetic data generation, and evolving regulatory frameworks. Strategic, phased adoption, coupled with a steadfast commitment to ethical AI development and comprehensive staff training, will be paramount in realizing the full revolutionary potential of TriageIQ.
The Evolving Landscape of Healthcare Triage
Current Inefficiencies and Pressures in Traditional Triage
Healthcare systems globally face persistent challenges in managing patient flow and ensuring timely, appropriate care. Traditional triage methodologies, which often rely on subjective human judgment and anticipated resource utilization, frequently contribute to significant inefficiencies. Emergency departments (EDs), for instance, grapple with issues such as overcrowding and prolonged patient delays. This reliance on human assessment can lead to both over-triage, where patients receive unnecessary attention, contributing to crowded EDs, potential infection exposure, and increased healthcare costs, and under-triage, where critically ill patients experience dangerous delays in care.
The sheer volume of patient interactions further exacerbates these pressures. In 2014, U.S. emergency departments alone recorded 141 million visits, a number that continued to grow, placing immense strain on existing infrastructure and personnel. Compounding this, chronic staffing shortages across various healthcare roles—including nurses, doctors, and telecommunicators—lead to high levels of stress and burnout among professionals. This, in turn, can compromise job satisfaction and increase the likelihood of errors, directly impacting patient safety and care quality. The pervasive nature of these inefficiencies, which are not isolated incidents but deeply embedded structural weaknesses, creates a compelling, almost unavoidable, demand for transformative solutions. The current state of healthcare triage underscores a fundamental need for technological intervention to achieve systemic change, making the "revolutionizing" aspect of TriageIQ a response to this urgent imperative.
Defining AI and Generative AI in the Healthcare Context
Artificial Intelligence (AI) in healthcare broadly refers to computer programs designed to analyze vast quantities of patient information, including symptoms, medical history, vital signs, and diagnostic scans. By identifying patterns within this data, AI algorithms can predict clinical outcomes and support medical decision-making. This capability has long been a focus in healthcare, aiming to enhance efficiency and accuracy.
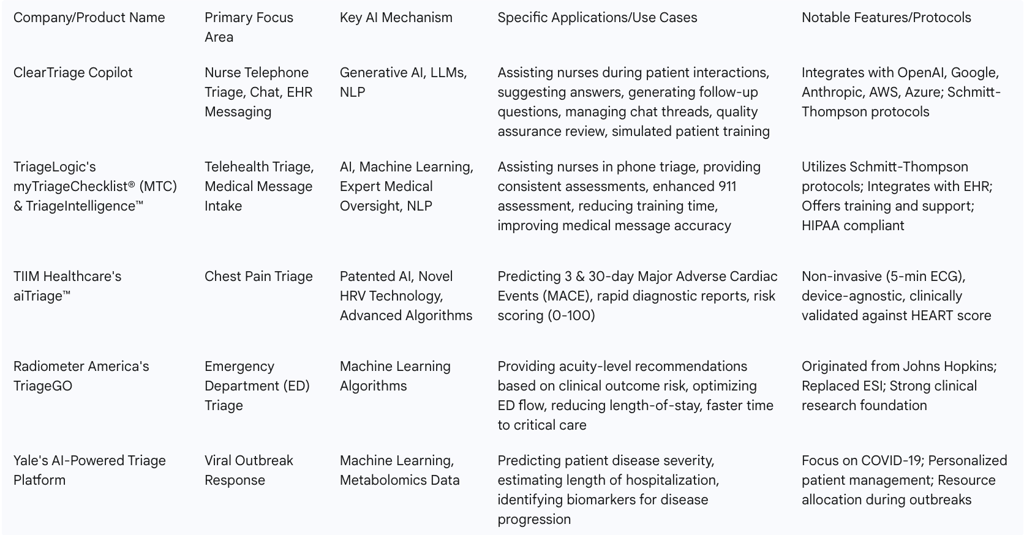
Generative AI (GenAI), however, represents a significant evolution within the AI landscape. Unlike traditional AI that primarily processes and analyzes existing data, GenAI models are capable of generating novel content. In the context of healthcare triage, this translates into advanced functionalities such as suggesting answers to triage questions, formulating intelligent follow-up inquiries, or summarizing extensive patient histories. Large Language Models (LLMs), a prominent subset of GenAI, are particularly relevant for conversational and text-based triage applications, enabling more natural and dynamic interactions. This shift signifies a qualitative leap: AI's role is moving beyond merely providing decision support to actively assisting in communication, documentation, and even training. For instance, systems like the ClearTriage Copilot function as front-line assistants, fundamentally altering the human-AI interaction model in triage by empowering human experts with intelligent tools rather than replacing their judgment.
The "TriageIQ" Paradigm: A New Era for Patient Management
The concept of "TriageIQ" encapsulates the intelligent and strategic application of AI to optimize patient assessment, prioritization, and resource allocation across the healthcare continuum. This paradigm is designed to address critical gaps, such as limited access to essential healthcare services for billions worldwide and the projected shortage of 11 million health workers by 2030. It marks a departure from traditional clinical decision tools, which have often demonstrated limited predictive accuracy, by leveraging AI's capacity for improved precision and data-driven insights.
The diverse applications of AI in triage, spanning from nurse telephone triage to emergency department flow optimization and specialized responses for viral outbreaks, illustrate that "TriageIQ" is not a singular product but a multifaceted strategic approach. Various companies and research initiatives are contributing to this ecosystem, including ClearTriage for nurse-led tele-triage , TIIM Healthcare's aiTriage for chest pain assessment , Radiometer America's TriageGO for ED acuity recommendations , and Yale's platform for viral outbreak response. This broad spectrum of applications, coupled with the systemic nature of existing healthcare challenges like overcrowding and staff burnout, indicates that for healthcare organizations, embracing "TriageIQ" necessitates the development of a comprehensive AI strategy. This strategy must integrate various AI tools across different triage points and workflows, rather than implementing isolated solutions. It requires a holistic vision for AI's role throughout the entire patient journey, from the initial point of contact to critical care management.
Core Mechanisms and Applications of AI in Triage
AI's integration into healthcare triage manifests through several core mechanisms, each designed to enhance specific aspects of patient management and operational efficiency.
AI-Powered Decision Support and "Copilot" Systems
A primary application of AI in triage involves providing intelligent decision support, often in the form of "Copilot" systems that augment human capabilities. The ClearTriage Copilot exemplifies this by assisting nurses during various patient interactions, whether on a call, in a live chat, or responding to an Electronic Health Record (EHR) message. This system leverages available patient data, such as transcriptions of initial assessments or results from symptom checkers, to suggest answers to triage questions. Nurses can then quickly confirm or reject these suggestions, enabling them to maintain focus on clinical decision-making while operating more efficiently. In chat-based interactions, the Copilot can also generate follow-up questions tailored to multiple parts of a triage protocol, maximizing the value of each inquiry and helping nurses manage multiple chat threads simultaneously, thereby improving both speed and safety.
Similarly, TriageLogic's myTriageChecklist® (MTC) and TriageIntelligence™ offer web-based solutions that integrate AI to support nurses in telephone triage. MTC provides consistent and accurate assessments by anticipating worst-case scenarios and guiding nurses on appropriate care levels—whether symptoms can be managed at home, by a Primary Care Provider (PCP), or require an Emergency Room (ER) visit. This system is built upon the widely recognized Schmitt-Thompson protocols, ensuring standardized guidelines for symptom evaluation. TriageIntelligence™ further integrates AI, machine learning, and expert medical oversight to deliver real-time insights, facilitate automated decision-making, and enable proactive care interventions, including enhanced 911 assessment capabilities. These systems primarily utilize Natural Language Processing (NLP) to interpret patient speech and notes, providing real-time support. The design philosophy behind these tools consistently positions AI as an augmentative force, emphasizing that AI should "enhance the triage process, not replace it," and always keep "the nurse's clinical judgment front and center". This approach, where AI suggests answers for nurses to "quickly confirm or reject" and TriageIntelligence incorporates "expert medical oversight" , is a critical design principle. It directly addresses potential user skepticism and ensures accountability by positioning AI as a powerful assistant that empowers human experts, rather than an autonomous decision-maker, thereby fostering trust and facilitating adoption.
Predictive Analytics for Risk Stratification
Beyond real-time decision support, AI excels in predictive analytics, enabling sophisticated risk stratification that informs patient prioritization. TriageGO by Radiometer America is an AI-powered clinical decision support tool specifically designed to optimize ED triage. It employs machine learning algorithms to generate acuity-level recommendations for nurses, based on the predicted risk of various clinical outcomes such as in-hospital mortality, ICU admission, or emergency surgery. This tool has a robust foundation in clinical research, having originated from a federally funded collaboration at Johns Hopkins Hospital.
Another specialized application is aiTriage™ by TIIM Healthcare, which stands as the world's first AI-powered platform for chest pain triage. This system predicts the risk of 3- and 30-day Major Adverse Cardiac Events (MACE) within minutes, non-invasively, using a 5-minute ECG recording and novel Heart Rate Variability (HRV) technology. It provides a clear 0-100 risk score with corresponding low, medium, and high-risk labels to guide treatment decisions. Clinical validation studies indicate that aiTriage is comparable to or more accurate than the traditional HEART score, even without a troponin test. For viral outbreak response, a platform developed by Yale University researchers leverages machine learning and metabolomics data to predict patient disease severity and potential length of hospitalization, offering a personalized approach to patient management and resource allocation during public health crises. These systems analyze real-time data, vital signs, clinical history, and unique biomarkers to generate probabilities or risk scores for specific health conditions. This capability goes beyond traditional risk prediction by identifying subtle patterns and providing more accurate assessments. The observed trend towards specialization, with aiTriage focusing on chest pain using ECG and HRV and Yale's platform on viral outbreaks using metabolomics , illustrates how specialization and diverse data modalities significantly enhance predictive accuracy. The future of predictive AI in triage will likely feature a portfolio of highly specialized models, each optimized for particular conditions or patient populations, integrating multimodal data such as text, images, genomics, real-time vitals, and metabolomics. This specialization allows for higher accuracy and more precise risk stratification, leading to more targeted and effective interventions.
Enhancing Operational Efficiency and Quality Assurance
AI's utility extends significantly to improving the operational efficiency and quality assurance within healthcare settings. ClearTriage, for example, supports LLMs in reviewing call recordings or transcripts, scoring them against customizable benchmarks to pinpoint calls that require human review. This capability is particularly valuable for nurse leaders, who often find evaluating triage calls to be a time-intensive and scarce resource.
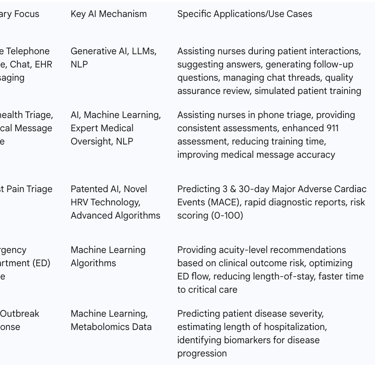
Furthermore, AI plays a crucial role in nurse training. ClearTriage, in combination with AI, allows new nurses to practice live conversations with simulated patients via voice or chat, with trainers able to select specific symptoms or diagnoses for the AI to emulate. Similarly, TriageLogic's TriageIntelligence aims to reduce the overall training time required for new nurses. By automating routine tasks and providing robust decision support, AI reduces the workload on triage nurses, leading to greater accuracy and efficiency in handling patient inquiries. AI can also assist in strategic resource planning by anticipating future call volumes, enabling more appropriate staffing of nurse call centers. Quantifiable improvements have been demonstrated by TriageGO, which has been shown to reduce the median length-of-stay in the ED by 15 minutes, decrease the median time to ICU or OR by 84 minutes, and lower the median time-to-hospitalization by 92 minutes. Beyond individual patient interactions, AI also enhances communication and transfer services, as evidenced by Conduit Health Partners' use of AI to centralize and automate stroke patient transfers, which reduced paperwork and alleviated staff burnout. The benefits of AI in triage extend beyond individual patient interactions to systemic improvements in quality assurance, training, workload management, resource planning, and inter-departmental communication. The significant operational impacts demonstrated by metrics from TriageGO underscore that AI in triage is not merely a clinical tool but a powerful lever for systemic operational transformation. It streamlines workflows, optimizes resource utilization, reduces staff burnout, and improves overall system responsiveness, positioning it as a strategic investment for healthcare administrators aiming to enhance efficiency and reduce costs across the entire organization.
Table 1: Overview of Leading AI Triage Solutions and Their Focus Areas
4. Transformative Benefits: Impact on Patient Care and Operations
The integration of AI into healthcare triage yields a multitude of benefits, profoundly impacting both the quality of patient care and the efficiency of operational workflows.
Improved Diagnostic Accuracy and Patient Safety
AI algorithms possess a remarkable capacity to analyze vast amounts of patient data, enabling them to identify subtle patterns that human clinicians might inadvertently overlook. This capability directly translates into improved diagnostic accuracy. AI systems provide consistent and clear risk scores, which helps to reduce human error and ensures standardized assessments across different patient interactions. For example, AI software has been demonstrated to be twice as accurate as human professionals in interpreting brain scans for stroke patients. Furthermore, AI can identify more bone fractures than humans and detect early signs of over 1,000 diseases, acting as a powerful diagnostic aid. The enhanced 911 assessment capabilities embedded within AI platforms further bolster patient safety by assisting nurses in identifying potentially life-threatening situations during telephone interactions. These capabilities position AI in triage as a crucial safety net and an effective early warning system. Its ability to detect subtle indicators , improve diagnostic precision , and flag critical conditions goes beyond mere efficiency; it directly influences patient outcomes by identifying issues that might otherwise be missed or by providing earlier, more precise risk assessments, which can be life-saving.
Enhanced Efficiency and Resource Optimization
AI significantly streamlines healthcare workflows, automates routine tasks, and provides robust decision support, thereby reducing the workload on triage nurses and leading to greater accuracy and efficiency in handling patient calls. This technological assistance is instrumental in managing emergency department overcrowding and mitigating delays by accurately prioritizing patients, resulting in shorter wait times and more precise patient prioritization. The quantifiable benefits are substantial: TriageGO, for instance, has demonstrated a median 15-minute reduction in ED length-of-stay, an 84-minute reduction in time to ICU or OR for critical patients, and a 92-minute decrease in time-to-hospitalization. Beyond immediate patient flow, AI can also optimize resource planning by accurately anticipating future call volumes and staffing requirements for nurse call centers. The improvements observed are not merely additive but create a multiplicative effect on healthcare operations. For example, a reduction in ED length-of-stay frees up beds and staff, allowing more patients to be seen. Faster time to critical care not only improves immediate patient outcomes but can also reduce long-term care costs. Automating routine tasks directly alleviates staff burnout , enabling healthcare professionals to dedicate their expertise to more complex cases. This illustrates that AI in triage offers a significant return on investment by optimizing the entire healthcare ecosystem, leading to lower operational costs, improved patient flow, and better utilization of scarce human and physical resources, ultimately making healthcare more sustainable and accessible.
Standardization of Care and Nurse Training
AI plays a pivotal role in promoting consistency and uniformity in healthcare delivery. By ensuring that all patients are assessed using standardized formats and evidence-based protocols, such as the widely recognized Schmitt-Thompson protocols , AI helps to reduce variability in care. This standardization is particularly crucial for large hospital networks striving to maintain consistent care quality across their various facilities. Furthermore, AI-powered training tools offer significant advantages for workforce development. ClearTriage's simulated patient conversations, for instance, provide a realistic environment for new nurses to practice live interactions, thereby enhancing their clinical experience and coaching. This method also contributes to reducing the overall training time required for new nurses. The ability of AI to enforce standardization directly addresses inconsistencies that can arise from subjective human judgment in high-pressure triage environments. Simultaneously, the provision of safe, scalable training environments through simulations is critical given the ongoing staff shortages in healthcare. This demonstrates that AI serves as a powerful catalyst for both quality improvement and workforce development. It helps organizations achieve a higher, more consistent quality of care and accelerates the onboarding and competency development of new nurses, thereby indirectly contributing to addressing the broader healthcare worker shortage and enhancing overall staff readiness.
Table 2: Quantifiable Benefits of AI in Triage
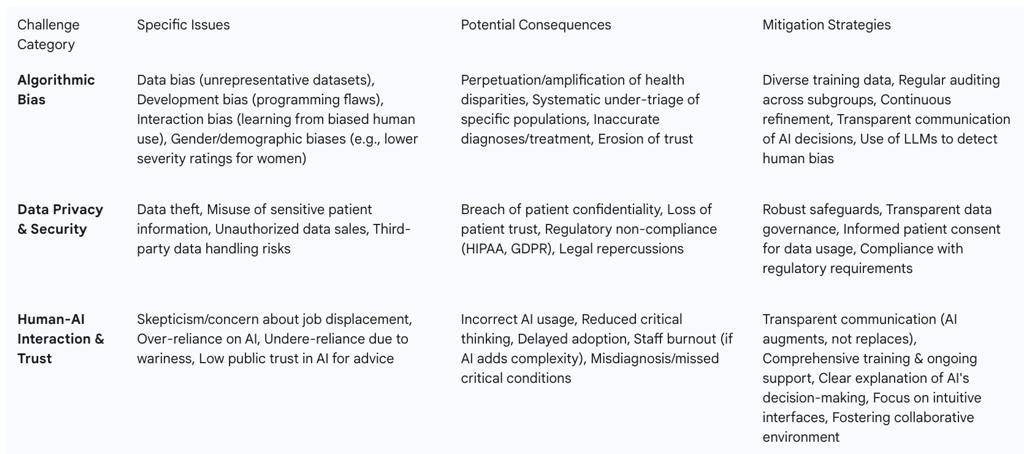
Challenges, Limitations, and Ethical Considerations
While the transformative potential of AI in healthcare triage is immense, its implementation is accompanied by significant challenges, limitations, and ethical considerations that must be proactively addressed.
Addressing Bias and Fairness in AI Algorithms
A critical concern in AI development is the potential for algorithmic bias. AI systems learn from vast datasets, and if these datasets are incomplete, unrepresentative, or reflect existing societal biases, the AI can inadvertently perpetuate or even amplify those biases. Research has indicated that AI models can reproduce caregiver biases, for instance, by assigning lower severity ratings to female patients compared to male patients presenting with identical clinical conditions. One study found that, based on identical clinical records, the severity of conditions for women tended to be underestimated (with approximately 5% classified as "less critical"), while for men, severity was slightly overestimated (3.7% deemed "more critical" versus 2.9% "less critical"). Such biases can be linked to demographic factors including sex, gender, age, and ethnicity, potentially leading to systematic under-triage of specific populations and exacerbating existing health disparities. It has also been observed that the level of inexperience in human staff can correlate with increased bias in AI models trained on their data, suggesting a feedback loop where human biases are encoded and potentially magnified by AI.
This dynamic reveals a critical recursive problem: AI learns from human data, and if human data contains biases, the AI will reproduce them, meaning AI doesn't just possess bias, but reflects and potentially magnifies existing systemic human biases in healthcare. Addressing this requires a multi-pronged approach. Mitigation strategies include ensuring diverse training data, conducting regular auditing of algorithm performance across various population subgroups, and continuous refinement of models. Interestingly, large language models (LLMs) themselves show promise in being able to detect and anticipate human cognitive biases, offering a potential tool for self-correction within AI development. Therefore, addressing bias is not a post-deployment fix but a fundamental requirement for ethical AI development, demanding proactive strategies that include diverse data collection, continuous auditing, and the use of AI itself as a tool for bias detection. Failure to do so risks exacerbating health disparities and undermining public trust in AI systems.
Data Privacy, Security, and Regulatory Compliance
Healthcare data is inherently sensitive, containing highly personal details, which makes patient privacy and trust paramount in any AI implementation. The integration of AI introduces risks such as data theft, misuse, and unauthorized sales, particularly when AI systems interact with data outside traditional secure systems or involve third-party AI tool providers. Strict compliance with established regulations like the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. and the General Data Protection Regulation (GDPR) in the EU is essential for safeguarding patient information and ensuring that informed consent is obtained for data usage. Patients must have a clear understanding of and explicitly agree to how AI utilizes their data, encompassing its role in diagnoses, treatment planning, and any data sharing practices. The emphasis on regulations like HIPAA and GDPR highlights that legal compliance is merely a baseline; the deeper issue revolves around establishing and maintaining patient trust. If patients lack confidence in how their sensitive data is handled, the widespread adoption of AI will be severely impeded, regardless of its clinical benefits. This means that robust data protection measures and transparent data governance frameworks are not merely regulatory hurdles but strategic imperatives for successful AI implementation. Building and maintaining patient trust through clear communication about data usage and strong security protocols is critical for the widespread acceptance of AI in healthcare.
The Imperative of Human Oversight and Trust in AI
The introduction of AI into healthcare can evoke skepticism among professionals, who may express concerns about their roles being diminished or even replaced. There is a dual risk: end-users might either be overly wary of new tools, leading to underutilization, or conversely, rely too heavily upon them, potentially resulting in incorrect usage or a loss of critical thinking. While AI demonstrates impressive capabilities, such as detecting two-thirds of missed issues like epilepsy lesions, it is acknowledged that a significant portion (one-third) remains difficult for AI to identify, underscoring the enduring necessity of human oversight and clinical expertise. Public trust in AI for providing basic health advice remains relatively low, with only 29% expressing comfort, although a higher proportion (over two-thirds) are comfortable with AI being used to free up professional time.
Addressing these concerns requires transparent communication, clearly articulating how AI will augment existing roles rather than diminishing or replacing them. Comprehensive and ongoing training and support for staff are crucial to ensure effective and appropriate use of AI technology. The challenges of overcoming human skepticism and preventing over-reliance on AI highlight a dual problem in human-AI collaboration, often referred to as the "last mile" problem of adoption and correct usage by frontline staff. The low public trust also indicates a broader societal challenge that extends beyond the clinical setting. Therefore, successful AI integration demands not only technological development but also substantial change management, education, and cultural shifts within healthcare organizations. It necessitates designing intuitive interfaces, providing thorough training, and fostering a collaborative environment where AI is perceived as a trusted partner, not a competitor or an infallible oracle.
Table 3: Key Challenges and Ethical Considerations in AI Triage
The Future Trajectory of GenAI in Healthcare Triage
The evolution of Generative AI in healthcare triage is poised to usher in an era of unprecedented capabilities, driven by advancements in AI models, data management, and a maturing regulatory landscape.
Emerging Trends: Multimodal AI, Synthetic Data, Personalized Medicine
The future of AI in healthcare will witness a significant shift towards multimodal AI models. These advanced systems will be capable of analyzing and generating content across various data modalities simultaneously, including text, images, genomics data, and real-time patient vitals. This integration of diverse data streams promises to significantly improve diagnostics and enhance clinical decision support by providing a more comprehensive understanding of a patient's condition.
Concurrently, the generation of synthetic data by GenAI will become a critical tool, especially given increasing concerns about patient privacy. This approach allows researchers to create realistic yet anonymous datasets for AI model training and research, thereby accelerating the development of new treatments without compromising patient confidentiality. Furthermore, GenAI technologies will play a pivotal role in advancing personalized medicine. By analyzing individual patient data, including genomics, lifestyle factors, and ongoing health information, these AI systems will tailor treatments and monitoring plans to specific patient needs. This capability contributes to improved patient compliance with treatment regimens and a reduction in medical errors. Beyond triage, AI will continue to drive breakthroughs in precision medicine, accelerating drug discovery by designing novel drug compounds in real-time and advancing diagnostics. The convergence of multimodal AI, synthetic data, and personalized medicine capabilities is not a set of isolated trends but a synergistic development. Multimodal inputs will allow for a complete patient picture, synthetic data will address privacy concerns for training these complex models, and personalized medicine will leverage this comprehensive data to deliver highly tailored care. This indicates that the future of TriageIQ is moving towards hyper-personalized, proactive care, where AI will not merely triage symptoms but predict disease progression, tailor interventions, and even accelerate drug discovery, fundamentally shifting healthcare from reactive to predictive and preventive models.
Regulatory Evolution and Collaborative Development
The landscape for AI in healthcare is rapidly maturing, marked by an increasing focus on regulatory frameworks. While 2024 saw the initial introduction of AI regulations, 2025 is expected to concentrate on refining these frameworks to ensure transparency, mitigate bias, and enhance data security. This will necessitate compliance with stricter policies, particularly in sensitive areas like clinical trials and drug development, where synthetic data generation will play a crucial role. Despite the rapid technological advancements, the healthcare industry's adoption of AI has been "below average" compared to other sectors. This highlights a significant opportunity for widespread implementation and a strategic transformation that extends beyond merely adopting new tools. Recognizing this, companies like ClearTriage are actively seeking partnerships with healthcare organizations to collaboratively explore and implement advanced AI capabilities. This collaborative development model, coupled with the refining regulatory environment, indicates a maturing AI healthcare ecosystem. The "below average" adoption also implies substantial growth potential as these frameworks solidify. The future will therefore be characterized by a more structured and regulated environment for AI in healthcare, fostering greater trust and accelerating adoption. This will likely lead to the development of more robust, interoperable solutions, forged through strategic partnerships between technology providers, healthcare organizations, and regulatory bodies.
Recommendations for Strategic Implementation
To effectively harness the transformative potential of AI in healthcare triage, strategic implementation must be guided by a phased approach and a strong commitment to ethical development.
Phased Adoption and Pilot Programs
For successful AI implementations in healthcare, it is highly recommended to begin with targeted pilot projects. These initial projects should focus on well-defined problems, such as improving triage accuracy for specific patient populations or accurately predicting daily staffing requirements. This incremental approach allows for careful evaluation of results and iterative refinement of the systems before broader, organization-wide deployment. This strategy directly addresses the inherent risks and potential skepticism associated with integrating new technologies. By starting small, organizations can conduct controlled testing, learn from real-world application, and adapt their approaches. This iterative learning process minimizes disruption to existing workflows, allows for continuous improvement based on actionable data, and gradually builds internal confidence and expertise within the organization before scaling the solutions.
Prioritizing Ethical AI Development and Training
A foundational element for successful AI integration is a steadfast commitment to ethical AI development. This includes transparent communication about how AI will augment, rather than diminish or replace, human roles within the healthcare team. Robust safeguards must be implemented to protect sensitive patient information, ensuring privacy while still leveraging the analytical value of the data. Continuous training and comprehensive support for staff are crucial to ensure they can effectively and confidently utilize AI technology. Furthermore, to mitigate bias and ensure equitable outcomes, it is imperative to use diverse training data, regularly audit algorithm performance across all population subgroups, and continuously refine AI models. The ethical considerations, encompassing bias, privacy, and human trust, are not merely compliance issues but are fundamental to successful adoption and public acceptance. Organizations that proactively address these concerns will build stronger trust with both patients and staff. Therefore, investing in ethical AI development, comprehensive data governance, and continuous staff education should be viewed not merely as a cost, but as a strategic investment. This approach differentiates organizations, fosters a culture of responsible innovation, and ultimately accelerates the widespread and beneficial integration of AI in healthcare triage.
FAQ Section
What is TriageIQ? TriageIQ is an advanced AI-based triage system designed to streamline patient assessment and prioritization in healthcare settings.
How does TriageIQ integrate with existing hospital systems? TriageIQ can be seamlessly integrated with existing hospital systems, including electronic health records (EHRs) and patient monitoring devices.
What are the key features of TriageIQ? Key features include real-time data analysis, integration with existing systems, decision support for clinical staff, specialized algorithms, and resource optimization.
How do AI-based triage systems improve emergency department integration? AI-based triage systems like TriageIQ analyze patient data to predict risks and recommend triage levels, reducing wait times and improving patient flow.
What is the role of AI in decision support for clinical staff? AI provides data-driven recommendations to support nurses and other clinical staff in making triage decisions, reducing subjective variability and ensuring appropriate care.
How do specialized algorithms enhance AI triage systems? Specialized algorithms tailored to specific conditions, such as stroke detection, enhance the accuracy of diagnosis and improve the timely dispatch of resources.
What are the benefits of AI in resource optimization for healthcare? AI decision support systems optimize the use of available resources, ensuring that patients receive the care they need, even in resource-limited settings.
What is the OlimpIA chatbot and how does it help victims of digital sexual violence? The OlimpIA chatbot provides legal advice and emotional support to victims of digital sexual violence, handling over 8,000 cases and offering tailored support.
How do Klineo and PatLynk use AI to match patients with clinical trials? Klineo and PatLynk use AI to analyze patient data and match it with trial criteria, accelerating the recruitment process for clinical trials and advancing medical research.
What future trends can we expect in AI-based healthcare triage? Future trends include enhanced data integration, advanced algorithms, and increased adoption of AI-based triage systems in healthcare settings.
Additional Resources
World Health Organization - For comprehensive information on global healthcare initiatives and guidelines.
American Medical Association - For insights into the latest medical research and healthcare policies.
Healthcare Information and Management Systems Society (HIMSS) - For updates on healthcare technology and innovation.
