Training Methodologies for Military Triage under Combat Stress
Military triage training is differentiated from civilian models by a core ethical and operational philosophy rooted in resource scarcity and mission focus. This framework dictates standardized care protocols and specialized decision-making processes, particularly in Mass Casualty (MASCAL) scenarios.


Military triage training is differentiated from civilian models by a core ethical and operational philosophy rooted in resource scarcity and mission focus. This framework dictates standardized care protocols and specialized decision-making processes, particularly in Mass Casualty (MASCAL) scenarios.
Tactical Combat Casualty Care (TCCC) as the Standard of Care
Tactical Combat Casualty Care (TCCC), established by the Joint Trauma System (JTS), represents the evidence-based standard for prehospital combat casualty management globally. The training is systematically structured around three distinct phases of operational care: Care Under Fire, Tactical Field Care, and Tactical Evacuation Care (TACEVAC).
The core sequence for initial assessment and treatment is mandated by the MARCH/PAWS algorithm: Massive Hemorrhage; Airway; Respiration; Circulation; Head injury/Hypothermia; Pain; Antibiotics; Wounds; and Splinting. The emphasis on Massive Hemorrhage as the immediate priority (before Airway, unlike traditional civilian protocols) is a critical distinction, reflecting the high percentage of battlefield deaths from uncontrolled extremity bleeding. Hemorrhage control is addressed using the "Four Ds": Detect the source, apply Direct pressure, use Devices (tourniquets or hemostatic gauze), and Don't Dilute (employ hypotensive resuscitation to avoid thinning the blood or disrupting clots). The widespread adoption of TCCC and MARCH/PAWS across the armed forces was a direct response to empirical analysis of combat data, which identified hemorrhage and airway failure as the leading preventable causes of death. Therefore, the training is inherently adaptive, focusing intently on the rapid, prioritized intervention necessary for survival.
Furthermore, the expansion of the mnemonic to include PAWS—specifically Hypothermia, Pain, and Antibiotics—demonstrates an institutional adaptation to anticipated operational requirements, such as austere environments and delayed evacuation. These elements become vital for a casualty who must survive for 6 to 72 hours post-injury in a Prolonged Field Care (PFC) setting, signifying a doctrinal shift from immediate evacuation models to robust sustainment capabilities.
The Ethics of Battlefield Triage and Resource Allocation
Military triage is fundamentally a utilitarian practice, focused on achieving the "greatest good for the greatest number of casualties" and ensuring the "most efficient use of available resources". Historically, this principle dictated prioritizing the stabilization of those casualties who could be most quickly treated and returned to the line, thereby restoring fighting capability and contributing to the common objective of victory. Triage is recognized as a continuous process demanding informed judgment, knowledge, and courage, necessitating that the most capable and experienced health care provider available assumes the triage role.
This utilitarian ethic becomes most acute during a MASCAL situation, defined by NATO as a major incident that overwhelms the local medical capabilities. In such scenarios, training must prepare medical personnel for the controversial concept of reverse triage, where those with less severe injuries (T3/Minimal) may be prioritized for rapid stabilization and return to duty, sometimes at the expense of treating more seriously injured (T2/Delayed) personnel immediately.
The requirement for medics to adopt such a severe utilitarian standard while operating under extreme physical and psychological pressure creates a profound ethical and cognitive burden. Training must specifically address this potential cognitive dissonance, ensuring personnel are prepared to execute complex prioritization decisions, including the T4/Expectant classification, accurately and professionally, a task far exceeding the typical ethical demands of civilian trauma care.
NATO Standardization and MASCAL Categorization (AMedP-1.10)
NATO doctrine, specifically AMedP-1.10, provides standardized categories for MASCAL triage, ensuring interoperability among allied forces. Casualties are assigned to one of four groups, often color-coded : T1 (Immediate/Red), T2 (Urgent/Yellow), T3 (Minimal/Green), and T4 (Expectant/White).
T1 casualties require immediate life-saving intervention or surgery, such as massive hemorrhage control or chest decompression, as they have the highest chance of survival with minimal resource expenditure. T3 casualties have relatively minor injuries and can usually care for themselves or be assisted by basic first-aid trained personnel. The T4 (Expectant) category consists of those casualties who are expected to die given the severity of the incident and the limited available resources. T4 status is reserved strictly for MASCAL situations and requires authorization at a strategic level; these patients receive only supportive and palliative care, preventing the diversion of finite resources from salvageable T1 or T2 patients.
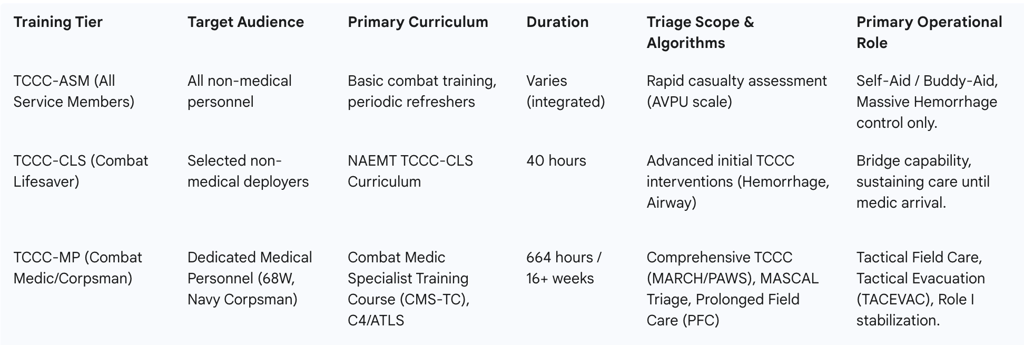
Training Continuum: Proficiency Tiers and Curriculum Requirements
Military medical training follows a standardized, tiered approach rooted in the TCCC doctrine, ensuring a wide distribution of critical life-saving skills across the entire force structure, from the frontline rifleman to the professional medical officer. This layering provides medical coverage across the operational spectrum.
A. TCCC for All Service Members (TCCC-ASM)
TCCC-ASM is the foundational tier, mandatory for all non-medical military personnel. This training focuses on the essential skills required for Self-Aid and Buddy-Aid at the immediate Point of Injury (POI). The assessment tools for non-medical personnel are simplified and reliable, such as the use of the Alert, Verbal, Pain, Unresponsive (AVPU) scale for determining a casualty’s mental status, rather than more complex evaluations like the Military Acute Concussion Evaluation (MACE), which is reserved for medical personnel. The curriculum’s core objective is the rapid assessment and control of massive hemorrhage, primarily through the application of limb tourniquets, which constitutes the most critical intervention for this tier.
B. The Combat Lifesaver (CLS) Program
The TCCC Combat Lifesaver (TCCC-CLS) course represents the second tier, a mandatory 40-hour program designed for selected non-medical military personnel deploying into combat zones. The CLS role is pivotal, acting as a bridge capability between the basic Self-Aid skills of the ASM and the advanced care provided by the professional medic. CLS training employs a systematic approach that includes achieving fire superiority, moving the casualty, conducting a structured assessment, performing treatment, and coordinating evacuation. Their expanded scope of practice includes using CoTCCC-recommended limb and junctional tourniquets and applying hemostatic dressings for compressible hemorrhage not amenable to tourniquet use. Standardization is ensured by requiring instructors to demonstrate comprehensive knowledge and skills across the specific TCCC tiers they teach. The strategic design of having these layered proficiency tiers (ASM, CLS, MP) demonstrates a doctrinal commitment to distributed medical capacity. This layering maximizes the survival rate during the critical initial minutes, ensuring that life-threatening interventions (the first steps of MARCH) can be performed immediately by the soldier closest to the injured, regardless of medical specialty.
C. The Combat Medic Specialist (CMS) and Medical Officer Training
The highest tier of prehospital training focuses on the professional medical provider, such as the Army Combat Medic Specialist (68W), who undergoes 664 hours of intensive instruction over 16 weeks at the Medical Education and Training Campus (METC). The curriculum requires successful completion of the National Registry Emergency Medical Technician (NREMT) cognitive assessment and practical validation, which ensures that foundational skills align with rigorous civilian trauma standards and facilitates interoperability. This specialized training integrates technical expertise with tactical skills, featuring a continuous 72-hour combat simulation scenario and an introduction to Prolonged Field Care (PFC).
Medical officers, including Physicians, Physician Assistants (PAs), and Nurses, receive specialized education through courses like the Combat Casualty Care Course (C4) and Advanced Trauma Life Support (ATLS). C4 specifically focuses on enhancing readiness for Role I and Role II operations, utilizing complex, mission-oriented scenarios such as MASCAL events and Military Operations on Urban Terrain. Advanced skills covered in these courses include shock management, thoracic trauma (including chest decompression), head and spine trauma management, and specialized surgical skills for trauma exposure (ASSET). The inclusion of dedicated PFC training addresses the requirement to manage stabilized casualties for approximately 6 to 72 hours in austere environments without immediate surgical capabilities. This heavy emphasis on sustained care is a clear doctrinal adaptation to the anticipated challenges of Large Scale Combat Operations (LSCO), where evacuation routes may be delayed or denied.
Table II: Comparison of Core US Military TCCC Training Tiers
Psychological Conditioning and Performance Under Fire
The unique challenge of combat triage lies not only in the technical difficulty of the interventions but in the cognitive difficulty of execution under extreme duress. Training must, therefore, actively condition personnel to maintain cognitive function and decision speed despite overwhelming psychological stimuli.
Cognitive Impacts of Combat Stress
Exposure to high task loads, time pressure, and the graphic nature of combat trauma are known to severely degrade cognitive processes. Stress alters attention, memory retrieval, and decision-making capabilities. An acute stress reaction can induce extreme sympathetic nervous system arousal, leading to impaired performance, such as "freezing" under fire, which directly prevents the execution of crucial life-saving measures. This failure in performance, coupled with the traumatic event, can increase the risk of longer-term psychological injury, including Posttraumatic Stress Disorder (PTSD). Since triage involves rapid classification and prioritization based on limited data (e.g., distinguishing T1 from T2 injuries), any performance degradation resulting from narrowed attention or cognitive impairment directly jeopardizes the accuracy of the decision, potentially leading to increased rates of lethal undertriage (missing critical wounds) or resource-wasting overtriage.
Stress Inoculation Training (SIT) Methodology
Stress Inoculation Training (SIT) is a core methodology used to prepare military personnel for highly stressful situations by diminishing potential negative psychological reactions. The method involves gradual, controlled, and repeated exposure to stress-related cues, which effectively desensitizes or "inoculates" the individual to panic responses, enabling them to execute complex tasks calmly and accurately in a stressful environment.
SIT is structured in three progressive stages :
Conceptual Education: Trainees are educated about expected cognitive and physiological reactions to stress (such as autonomic arousal) and introduced to basic mental skills, including visualization, self-talk, and confidence-building, which help optimize performance under duress.
Skills Acquisition and Consolidation: This phase involves learning and practicing problem-solving strategies and specific coping skills designed to manage physiological responses (e.g., breathing control, relaxation) and stop upsetting or paralyzing thoughts.
Application and Follow-Through: Trainees are exposed to progressively difficult and cumulative stressors, challenging them sufficiently without overwhelming their ability to perform the required technical skills.
High-Fidelity Field Exercises and Stressors
The application phase of SIT heavily relies on high-fidelity, live training exercises (LIVEX). These scenarios incorporate realistic combat conditions, including smoke, simulated artillery fire, and role-players whose severe injuries are replicated using prosthetic wound simulation, or "moulage," to enhance realism. Surprise mass casualty exercises (MASCAL) are often incorporated during annual training to specifically test and validate medical response systems, including casualty collection points, triage procedures, and evacuation timelines, under acute stress. The consistent focus on realism and the deliberate induction of stress during these exercises ensures that the inoculation is effective and that the skills learned transfer successfully to real-world combat environments. This focus is also recognized as a key component in the primary prevention of PTSD, as fostering optimal performance and resilience during critical moments contributes directly to long-term psychological health.
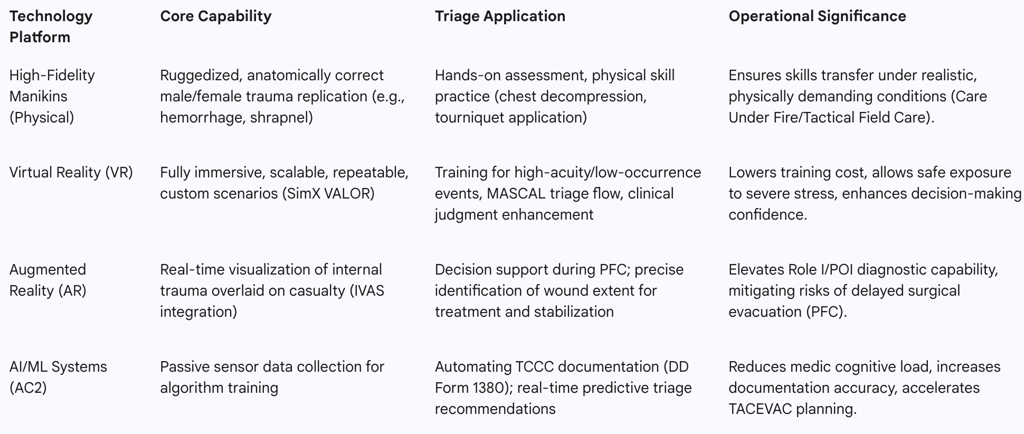
Advanced Simulation Technologies for Triage Mastery
The armed forces employ a sophisticated spectrum of simulation technologies, ranging from ruggedized physical manikins to advanced digital environments, to provide repeatable, measurable, and highly realistic training for complex triage scenarios.
High-Fidelity Physical Simulation Systems
Physical simulators are designed to replicate the complexity of combat trauma and the physical demands of field care. Training centers utilize ruggedized, full-body manikins, such as the Rescue Randy series and trauma simulation manikins, capable of mimicking severe burn, shrapnel, and bullet wounds through wearable attachments. These mannequins are specifically engineered to be durable enough to withstand the demanding conditions of training lanes, which simulate tactical movement, care under fire, and casualty evacuation (e.g., buddy-dragging a casualty for 50 meters). A critical aspect of maintaining high fidelity is ensuring anatomical accuracy, exemplified by the fielding of anatomically correct female manikins. This is necessary to prevent any potential hesitation or error caused by unfamiliarity on the battlefield when treating female casualties.
Virtual Reality (VR) and Serious Games
Virtual Reality platforms, such as SimX VALOR, offer a scalable and accessible alternative to traditional field exercises. VR provides fully immersive, repeatable, and customizable scenarios for battlefield triage, trauma treatment, and tactical evacuation. By immersing learners in lifelike situations that replicate the chaos and information overload of a combat zone, VR significantly enhances critical thinking and clinical judgment, particularly for high-acuity, low-occurrence events that are difficult to stage physically.
Digital training tools, often referred to as Serious Games (SGs), are also emerging as effective instructional platforms. Comparative trials have demonstrated that scenario-based SGs outperform traditional video-based online courses in improving both learning proficiency and trainee self-confidence regarding tactical combat casualty care skills.
Augmented Reality (AR) as a Triage and Decision Aid
Augmented Reality (AR) technology is being developed to integrate sophisticated diagnostic support directly into the combat environment. Projects are leveraging AR headsets, such as the Army's Integrated Visual Augmentation System (IVAS) goggles, to overlay high-fidelity visualizations of internal anatomy and realistic trauma onto the injured Warfighter. The objective is to provide a real-time decision support tool during triage and Prolonged Field Care (PFC). This technology acts as a force multiplier, mitigating the risk of delayed surgical evacuation by allowing medics at the Point of Injury (POI) to visualize the location and extent of internal wounds, akin to having CT-scan diagnostic capability in the field, optimizing stabilization and resource utilization during the extended casualty management window.
International Simulation and Policy Validation (NATO)
The integration of modeling and simulation (M&S) extends beyond individual skill practice to strategic policy validation. NATO, through its Centre of Excellence for Military Medicine in Budapest, Hungary , utilizes computer simulators (SIMEDIS) during large-scale exercises, such as Vigorous Warrior/Clean Care. These tools model complex tactical scenarios and quantify the impact of shifts in evacuation timelines and resource scarcity on medical outcomes for Large Scale Combat Operations (LSCO). This systematic approach supports Concept Development and Experimentation (CD&E) and aids in refining battlefield medical planning. However, NATO analysis recognizes a critical need for continued validation studies and the establishment of standardized metrics to accurately assess the learning and skill improvement derived from these M&S technologies.
Table III: Advanced Simulation Technologies and Triage Application
Metrics, Evaluation, and Quality Improvement
To ensure that training efficacy translates directly into combat effectiveness, military organizations employ rigorous measurement protocols, assessing not only technical skills but also the speed and accuracy of critical triage decision-making under stress.
Assessing Triage Performance: Metrics and Standards
The effectiveness of triage training is primarily quantified using key performance indicators (KPIs): triage time (speed), accuracy (correct categorization), overtriage rate (allocating excessive resources), and undertriage rate (failing to identify a critical injury). Simulation studies comparing triage systems show that simplicity often correlates with speed, a critical factor in MASCAL events. For instance, the START system can be completed significantly faster than more complex systems (e.g., 33 seconds per patient) while maintaining a comparable level of accuracy.
A recognized challenge in performance evaluation is the difficulty in specifying precise criteria and standards for tactical decision-making due to the unpredictable nature of combat scenarios. This highlights that combat triage is not a purely medical task; it is fundamentally integrated into mission tactics. Evaluation must, therefore, assess both medical competence and sound tactical judgment, which necessitates the development of specialized assessment tools that provide substantive, quantifiable data on a trainee’s performance.
Continuous Quality Improvement through Simulation Data
Continuous quality improvement (CQI) is achieved through the rigorous collection and analysis of data generated during large-scale exercises. Multinational LIVEX events, such as those conducted by NATO (Vigorous Warrior), involve meticulously collecting quantitative and qualitative data regarding medical performance from the point of injury (PoI) up to Role 2 facilities. This field data, focused on triage, damage control resuscitation, and surgery, is then used to recreate scenarios and refine computer simulation models like SIMEDIS. The use of simulators and subsequent debriefing reports is directed toward all NATO partners, establishing a collaborative mechanism for validating best practice standards and refining medical policy, particularly for LSCO. This commitment to international data sharing is essential for generating standardized, high-quality datasets to predict future combat medical requirements.
The simulation environment provides a controlled setting to test the critical relationship between resource scarcity and decision accuracy. When resource constraints are introduced into MASCAL scenarios, the resulting utilitarian pressure increases the cognitive burden on the provider, which correlates with measurable decreases in accuracy, such as increased undertriage rates. Measuring this relationship allows trainers to identify and mitigate performance degradation points. Furthermore, ongoing research efforts aim to develop metrics that can objectively measure how induced psychological stress impacts cognitive control during these simulated triage situations , thereby completing the feedback loop between Stress Inoculation Training (SIT) and quantifiable performance.
The Future of Autonomous and Distributed Casualty Care
The future of military triage training and execution is centered on integrating machine learning and autonomy to enhance decision speed, reduce cognitive burden, and ensure better outcomes in increasingly complex operational environments.
Passive Data Collection and Autonomous Documentation (AC2)
The Autonomous Casualty Care (AC2) research portfolio addresses the historical challenge of accurately and consistently capturing TCCC data in operational settings. The current research effort, Passive Data Collection using Autonomous Documentation, employs systematic, simulated TCCC scenarios using both high-fidelity manikins and live simulated patients.
Care providers and simulated patients are equipped with suites of passive sensors that collect detailed data on clinical actions and physiological changes. This data (with a goal of annotating 2500 initial procedure tasks) is used to train Machine Learning (ML) and Artificial Intelligence (AI) algorithms. The goal is the autonomous population of critical medical forms, such as the Department of Defense (DD) Form 1380, which significantly reduces the administrative cognitive load on combat medics. By offloading non-clinical tasks, the medic is freed to dedicate more attention to rapid clinical decision-making and patient care, which is expected to measurably enhance triage speed and accuracy.
AI-Driven Triage and Predictive Analytics
AI-driven triage systems represent a groundbreaking technological development in prioritizing and managing injuries on the battlefield. These systems leverage machine learning algorithms and data analytics to rapidly process vast amounts of medical data, assess injury severity, and predict outcomes. They provide instant recommendations to medical personnel, which is vital when every second counts in a high-pressure combat situation. The AI’s ability to simulate various intervention pathways allows medics to quickly determine the most effective course of treatment and whether a casualty requires immediate evacuation or can be managed on-site.
The development of sophisticated AR/IVAS systems and integrated AI decision support requires a corresponding evolution in medical training. Future training must focus on human-AI team performance, teaching medics how to effectively integrate, trust, and critically evaluate the real-time, data-driven recommendations provided by autonomous systems, thereby adding a new layer of technological and cognitive proficiency to TCCC practice.
Distributed Technology Enhancements
Innovations are also driving decentralized and enhanced tracking capabilities. Digital Triage Tags are being developed to streamline categorization and enable real-time tracking of casualties, which improves situational awareness and accelerates medical intervention and coordination during MASCAL incidents. Furthermore, programs like the DARPA Triage Challenge are focused on driving innovations in identifying vital signs of injury, locating and assessing casualties, and rapidly transmitting critical data to responders, ensuring care prioritization when medical resources are scarce. The passive data collection methods used in AC2 are designed to directly feed the AI algorithms used in operations, creating a closed-loop system where simulation data continuously refines the autonomous tools utilized in distributed casualty care.
Conclusions
Military training for rapid triage under combat conditions is a highly evolved, layered system driven by the utilitarian principle of maximizing salvageable lives under conditions of resource scarcity and extreme duress. The training doctrine is anchored by the evidence-based Tactical Combat Casualty Care (TCCC) guidelines, utilizing the MARCH/PAWS algorithm to prioritize immediate, life-saving interventions, primarily hemorrhage control.
Training success is ensured through a tiered proficiency structure, ranging from TCCC-ASM (universal basic care) to the advanced, NREMT-certified Combat Medic Specialist (MP), who is specifically trained for Prolonged Field Care (PFC) in anticipation of denied or delayed evacuation in LSCO environments.
Crucially, performance preservation under stress is achieved via sophisticated Stress Inoculation Training (SIT), which uses high-fidelity physical manikins and advanced virtual reality (VR) and Serious Games simulations to induce and manage cognitive load, preventing decision paralysis and optimizing triage accuracy. The future trajectory of military medical readiness involves integrating Augmented Reality (AR) to bring near-diagnostic capability to the point of injury and deploying Autonomous Casualty Care (AC2) systems to automate documentation, thereby strategically relieving the medic's cognitive burden and enhancing clinical decision speed in chaotic environments. The continuous refinement of this ecosystem relies heavily on shared data from multinational live exercises and the validation of simulation metrics related to triage time and accuracy.
