Quantifying the Impact of AI Triage on Patient Outcomes
Explore groundbreaking 2025 research revealing how AI triage systems have revolutionised healthcare delivery, with data-driven insights on reduced wait times, improved diagnostic accuracy, and enhanced patient outcomes across diverse clinical settings.


Artificial intelligence (AI) powered triage systems are rapidly transforming healthcare, particularly in high-pressure environments like emergency departments. By leveraging advanced algorithms, machine learning, and natural language processing, these systems aim to enhance efficiency, accuracy, and patient outcomes. This report provides a comprehensive review of the quantifiable impacts of AI triage, examining its effects on clinical accuracy, patient flow, resource optimization, and both patient and clinician experience. While significant benefits such as reduced waiting times, decreased mis-triage rates, and improved clinician satisfaction have been demonstrated, challenges persist. These include methodological heterogeneity in research, technical issues like algorithmic bias and performance degradation, and human factors such as clinician trust and workflow integration. Ethical considerations, particularly around data privacy, transparency, and accountability, are also paramount. The analysis concludes that AI triage holds immense promise, but its full potential hinges on rigorous multi-center validation, the development of explainable AI, robust ethical frameworks, continuous clinician engagement, and adaptive regulatory oversight to foster a truly learning healthcare system.
1. Introduction: The Role of AI in Healthcare Triage
The integration of artificial intelligence into healthcare triage represents a pivotal advancement, offering sophisticated tools to navigate the complexities of modern patient care. This section establishes a foundational understanding of AI triage, its core functionalities, and the compelling reasons for its adoption in healthcare.
1.1. Defining AI-Powered Triage Systems
AI in triage leverages advanced algorithms and machine learning techniques to assist healthcare professionals in making informed decisions, with the overarching potential to enhance efficiency, accuracy, and patient outcomes. It embodies the broader concept of technology performing tasks in an autonomous and intelligent manner, with machine learning as a subset specifically focused on learning from data, identifying patterns, and making decisions with minimal human intervention.
These systems are meticulously designed to optimize patient assessment, streamline resource allocation, and refine clinical workflows, ultimately leading to faster time-to-treatment and elevated patient satisfaction. Their critical role is particularly pronounced in emergency medicine, where they are poised to accelerate triage, diagnosis, and prognostication through the sophisticated input of clinical information and advanced image recognition capabilities. The primary objectives driving the development and implementation of AI triage include improving the accuracy of initial assessments, significantly reducing patient waiting times, allocating scarce resources more efficiently, and optimizing the overall flow of patients within high-demand environments such as emergency departments. Beyond these direct benefits, AI also aims to streamline patient intake processes, alleviate bottlenecks within emergency departments (EDs), enhance the precision of clinical decisions through evidence-based algorithms, and contribute to lower administrative costs across healthcare organizations.
1.2. Key AI Technologies Utilized in Triage
A diverse array of AI technologies underpins the functionality of modern triage systems, each contributing unique capabilities to the assessment and management of patients.
Decision Support Systems: These AI applications analyze a wide spectrum of patient data, including vital signs, comprehensive medical histories, and reported symptoms. They provide crucial decision support to healthcare professionals, aiding in the rapid determination of a patient's condition urgency and suggesting appropriate interventions. Such systems are typically trained on extensive datasets of historical patient records, enabling them to inform their recommendations with a broad base of knowledge.
Predictive Analytics: Leveraging large volumes of historical patient data, AI algorithms in this domain identify intricate patterns to forecast patient outcomes. This includes predicting the likelihood of clinical deterioration or the necessity for specific medical interventions, considering a multitude of factors such as vital signs, laboratory results, and demographic information.
Image Analysis: In emergency departments, where medical imaging is indispensable for diagnosis and triage, AI-powered image analysis plays a transformative role. It facilitates the rapid interpretation of X-rays, CT scans, and other imaging modalities, efficiently identifying critical findings or abnormalities that demand immediate medical attention.
Natural Language Processing (NLP): NLP techniques are employed to extract pertinent information from unstructured patient narratives, such as medical history notes and chief complaints. AI-powered NLP models can summarize complex patient information, flag important details for clinicians, and provide robust support for the decision-making process. This technology also extends its utility to Health Technology Assessment (HTA) by automating and enhancing systematic reviews of medical literature.
Triage Chatbots and Voice Agents: AI-powered chatbots serve as initial points of contact, gathering preliminary patient information and offering guidance during the triage process. These chatbots assess symptoms and direct patients to appropriate levels of care based on the severity of their condition. More advanced voice agents, often incorporating Neuro-Symbolic AI (a paradigm combining Generative AI with probabilistic reasoning), can conduct structured pre-triage assessments, significantly reducing call durations and improving the quality of data collected before a human healthcare professional intervenes.
Resource Optimization: AI algorithms analyze real-time operational data, including patient flow, bed availability, and staffing levels within the emergency department. Based on this analysis, AI can suggest highly efficient patient assignment and workflow strategies, thereby reducing wait times and enhancing overall operational efficiency.
Data Augmentation and Remote Monitoring: The integration of AI systems with digital stethoscopes and other remote monitoring devices enables the capture of objective clinical data, such as heart and lung sounds or vital signs. This capability allows AI to continuously assess incoming patient-generated data, particularly valuable for chronic disease management, by flagging early signs of deterioration and prompting timely interventions.
1.3. The Imperative for AI in Modern Healthcare
The adoption of AI in healthcare triage is not merely an incremental improvement but a strategic imperative driven by the escalating pressures on healthcare systems worldwide. Emergency departments, in particular, face mounting challenges from increasing patient volumes, persistent overcrowding, and significant resource constraints. These factors collectively compromise the timely delivery of care and contribute directly to adverse clinical outcomes.
Traditional triage systems, while providing a structured approach, frequently rely on subjective assessments by human operators. This inherent subjectivity can lead to inconsistencies in patient prioritization, especially during peak hours or mass casualty events, where the volume and complexity of cases overwhelm human capacity. AI offers a compelling solution by automating patient prioritization through the rapid analysis of real-time data, thereby standardizing decision-making and reducing variability.
A fundamental shift in how AI is conceptualized in healthcare is evident: AI is increasingly viewed as a force multiplier rather than a direct replacement for human expertise. Multiple sources emphasize that AI is designed to "assist healthcare professionals" , "support decision-making" , and maintain a focus on "supporting—not replacing—the human touch". This recurring theme underscores a strategic design philosophy that recognizes the irreplaceable value of human clinical judgment. The implication is that successful and ethical integration of AI in healthcare triage depends on a symbiotic relationship where AI augments human capabilities. This requires implementation strategies that prioritize comprehensive training for healthcare professionals, enabling them not only to operate AI tools but also to critically interpret and validate AI-generated insights. This approach is crucial for building trust and ensuring that AI serves as a powerful assistant, enhancing rather than undermining, the clinician's role.
Furthermore, the very definition of "triage" is evolving with the advent of AI. While traditionally triage has been understood as an initial, episodic assessment , AI significantly expands this scope. References to "predictive analytics" , "risk stratification" , "population health and remote monitoring" , and "pre-triage voice agents" indicate that AI's role extends far beyond a single point-of-care evaluation. This suggests a transformation towards continuous and proactive patient management. The broader implication is that AI is reshaping triage from a static, episodic event into a dynamic, continuous process that can commence even before a patient physically arrives at a healthcare facility and extend throughout their entire care journey. This expanded conceptualization of "triage" opens new avenues for early intervention, chronic disease management, and remote care delivery. Consequently, the metrics used to quantify AI's impact must also broaden beyond traditional emergency department throughput measures to encompass long-term patient outcomes and system-wide efficiencies across the entire continuum of care.
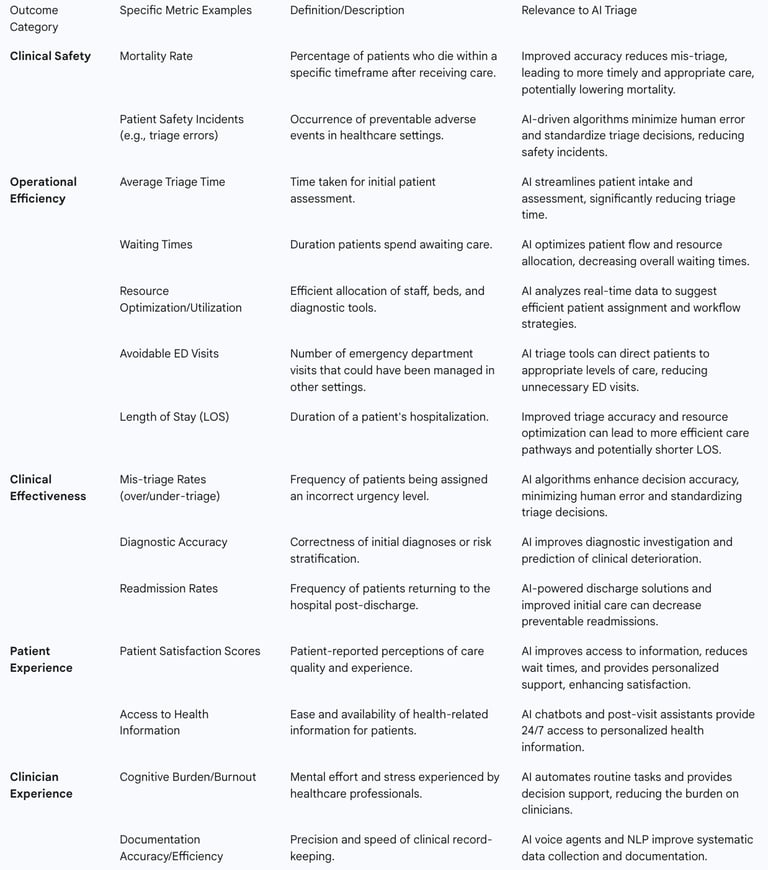
2. Defining and Measuring Patient Outcomes in Healthcare
To accurately quantify the impact of AI triage, it is essential to establish a clear understanding of what constitutes a "patient outcome" in healthcare and how these outcomes are measured. This section delineates the critical categories of patient outcomes and their relevance to AI interventions.
2.1. Comprehensive Categories of Patient Outcome Measures
Healthcare outcome measures are fundamental for assessing the quality and effectiveness of care, serving as results-oriented indicators that reflect the ultimate impact of medical interventions. The most common and critical categories of outcome measures include:
Mortality: This metric reflects the percentage of patients who die within a specific timeframe after receiving care. It is an essential population health outcome measure, widely used to assess the effectiveness of healthcare interventions and the overall quality of care provided. For example, evidence-based care standardization for pneumonia patients at Piedmont Healthcare resulted in a notable 56.5% relative reduction in the pneumonia mortality rate.
Readmissions: This measure quantifies the frequency with which patients return to the hospital within a defined period following discharge. High readmission rates often indicate inadequate discharge planning or insufficient post-discharge support, and they represent a significant financial burden as they are frequently preventable. The University of Texas Medical Branch (UTMB), for instance, achieved a 14.5% relative reduction in their 30-day all-cause readmission rate by implementing care coordination programs and leveraging analytics. AI-powered digital discharge solutions are specifically noted for their potential to decrease readmission rates, linking directly to improved hospital performance and insurance reimbursement.
Safety of Care/Patient Safety Indicators: These measures pertain to the occurrence of preventable adverse events within healthcare settings. Common examples include falls, pressure ulcers, medication errors, and hospital-acquired infections (HAIs). The overarching aim of these measures is to enhance patient safety and minimize harm during healthcare delivery.
Effectiveness of Care: This category evaluates two key aspects: compliance with established best practice care guidelines and the achievement of desired clinical outcomes, such as lower readmission rates for specific conditions like heart failure. It underscores the importance of adhering to evidence-based care protocols to achieve optimal patient results.
Patient Experience/Patient-Reported Outcome Measures (PROMs): This category captures patients' subjective perspectives on their health status, quality of life, and overall satisfaction with the healthcare services they receive. PROMs offer a more realistic gauge of patient satisfaction and provide real-time information that can be used for immediate service improvement. Patient satisfaction is a frequently cited benefit of AI triage systems.
Timeliness of Care/Reduced Wait Times: This is a critical measure of operational efficiency and a significant determinant of patient satisfaction. It encompasses metrics such as average triage time and the overall efficiency of patient flow within a facility.
Efficient Use of Medical Imaging/Resource Optimization: This measure assesses how effectively resources, including diagnostic tools like medical imaging, are utilized. AI plays a crucial role in this area by aiding in the rapid interpretation of medical images and optimizing the allocation of various resources within the healthcare system.
Length of Stay (LOS): This refers to the duration of a patient's hospitalization. A longer LOS can indicate complications or inefficiencies in care delivery and directly impacts hospital resources and costs, making it a key measure of operational efficiency.
Functional Status Improvement: This metric measures changes in a patient's ability to perform daily activities after receiving treatment. It reflects the practical impact of care on a patient's quality of life and their capacity to return to normal functioning.
2.2. Quality Metrics and Their Relevance to AI Interventions
Quality metrics, also known as quality indicators, serve as indispensable tools in healthcare for evaluating the effectiveness, safety, and efficiency of patient care. They empower healthcare providers to track performance, pinpoint areas requiring improvement, and make data-driven decisions regarding staffing, equipment, and facility needs. These indicators can be broadly categorized into structural, process, clinical outcome, patient safety, patient experience, efficiency, and access/equity indicators. AI interventions directly influence several of these categories:
Process Indicators: AI systems streamline patient intake and assessment processes , directly enhancing the efficiency and standardization of clinical workflows.
Clinical Outcome Indicators: By improving diagnostic accuracy and reducing mis-triage, AI directly impacts clinical results, leading to more appropriate and timely interventions.
Patient Safety Indicators: AI's ability to minimize human error and standardize triage decisions can lead to a reduction in patient safety incidents related to triage.
Patient Experience Indicators: AI improves access to health information and significantly reduces wait times, thereby enhancing overall patient satisfaction.
Efficiency Indicators: AI optimizes resource allocation and patient flow, directly impacting the cost-effectiveness of healthcare services and the utilization rates of diagnostic tests.
The Donabedian Model, which evaluates healthcare quality based on structure, process, and outcomes, along with the Institute of Medicine's (IOM) six domains of healthcare quality (safe, effective, patient-centered, timely, efficient, and equitable), provide robust frameworks for assessing how AI triage contributes to overall healthcare quality.
A significant observation is the interconnectedness of operational efficiency and clinical outcomes. Multiple sources frequently link AI's operational benefits, such as "reduced waiting times," "optimized resource allocation," and "reduced ED bottlenecks" , with direct improvements in clinical quality, including "improved accuracy" and "reduced mis-triage rates". This suggests a causal chain where operational efficiencies serve as critical intermediate outcomes, directly enabling more timely and accurate clinical interventions, which are prerequisites for improved patient outcomes. The financial perspective also highlights the necessity for sustainable innovation, implying that operational savings can be reinvested to fund quality improvements. Therefore, a comprehensive quantification of AI's impact must adopt a holistic evaluation framework that integrates both operational efficiency metrics and clinical outcome measures. Operational improvements are not merely administrative benefits; they are fundamental to enhancing the quality and timeliness of care delivery, thereby indirectly but significantly impacting ultimate patient health outcomes. This broader perspective is essential for demonstrating the full value proposition of AI to financially constrained healthcare systems.
Furthermore, there is an increasing emphasis on patient-centered and experiential outcomes. While traditional healthcare evaluation often prioritizes clinical endpoints like mortality and readmissions, numerous sources highlight AI's positive impact on "patient satisfaction" , "patient experience" , and patient-reported benefits such as "24/7 access to health information" and "personalized discharge instructions". This indicates a growing recognition of the patient's perspective as a crucial outcome measure. As healthcare systems transition towards value-based care and patient empowerment, the "impact" of AI triage is increasingly defined by subjective patient experiences alongside objective clinical metrics. This necessitates that future AI development and evaluation explicitly incorporate patient preferences, accessibility, communication effectiveness, and satisfaction as core outcome measures. AI's ability to deliver measurable value in these areas can be a significant driver for adoption, even if its direct impact on "hard" clinical outcomes is more complex to isolate or slower to manifest.
Table 1: Key Patient Outcome Measures Relevant to AI Triage
3. Methodologies for Quantifying AI Impact in Clinical Settings
Quantifying the impact of AI in clinical settings demands rigorous methodologies that move beyond theoretical benefits to demonstrate tangible improvements in real-world practice. This section explores the established and evolving approaches to evaluating AI's influence.
3.1. Approaches to Clinical Evaluation of AI
The clinical evaluation of AI aims to confirm acceptable performance through adequate external testing and to validate the benefits of AI-assisted care when compared to conventional care. Appropriately designed and conducted studies are essential, with prospective studies being highly desirable for robust evidence generation.
One primary approach involves a comparative evaluation of diagnostic performance and patient outcomes between conventional, AI-unassisted practice and AI-assisted practice. This allows for direct assessment of the incremental value AI brings.
External testing is a crucial component of this evaluation, involving the assessment of an AI algorithm's performance using data collected independently from its development. This typically means using data from different institutions (geographic generalizability) or different time periods (temporal generalizability). A significant concern, however, is that many commercially available AI products lack rigorous scientific validation, with 64% having no peer-reviewed evidence and few demonstrating clinical impact beyond mere diagnostic accuracy. Furthermore, a review of FDA-approved medical AI devices revealed that a substantial number (93 out of 130) lacked multisite assessment in their evaluation studies, highlighting a gap in demonstrating broad applicability.
Paired designs offer substantial advantages for comparing performance between AI-unassisted and AI-assisted diagnoses, particularly when AI is integrated as an add-on tool to existing clinical workflows. These designs allow for direct comparison within the same clinical context.
Systematic reviews and meta-analyses are invaluable methodologies that synthesize findings from multiple studies to provide a comprehensive overview of AI's impact. For instance, a 2023 Journal of Medical Internet Research meta-analysis provided key insights into AI triage , and systematic reviews have specifically focused on AI-based triage systems in emergency departments. Integrative reviews also play a crucial role in synthesizing existing literature to identify trends and gaps.
Clinical trials, such as the cluster-randomized RAPIDx AI trial, are essential for rigorously evaluating AI tools in real-world settings. This trial, for example, investigated an AI-based clinical support tool for ED triage of suspected cardiac conditions, yielding critical insights into its impact on patient outcomes. Finally,
pilot programs represent smaller-scale implementations that allow for the testing, refining, and validation of AI systems within specific healthcare environments before broader deployment. Sanford Health's pilot program for AI-driven colon cancer screenings exemplifies this, where retrospective data was used to test effectiveness before a physician-led pilot was launched.
3.2. Importance of Measurable Clinical and Financial Outcomes
To effectively demonstrate the benefits of AI, particularly to stakeholders who may not yet be utilizing AI, the presence of clearly measurable outcomes is paramount. This is especially critical in the healthcare sector, where health systems often operate on exceptionally thin financial margins, typically in the single-digit percentage range, sometimes even below five percent. In such an environment, even when organizations are deeply passionate about improving care, they must identify sustainable innovation models. The ability to measure both clinical and financial value is therefore key to justifying investment and ensuring long-term viability.
AI-powered patient triage systems are explicitly designed to deliver measurable benefits for healthcare professionals and administrators. These benefits extend beyond clinical improvements to include tangible cost savings and enhanced operational efficiency, which directly contribute to the financial health of the organization. Quantifying this impact necessitates precise, data-driven insights. These insights are crucial for tracking performance against benchmarks, identifying specific areas for improvement, and making informed decisions regarding resource allocation and the overall delivery of care. Without clear, quantifiable results, the adoption and sustained investment in AI technologies in healthcare remain challenging.
3.3. Role of Health Technology Assessment (HTA) Frameworks in Evaluating AI
Health Technology Assessment (HTA) is a systematic, multidisciplinary evaluation of the clinical, economic, and social implications of health technologies. It plays a crucial role in informing critical decisions related to pricing, reimbursement, formulary inclusion, and broader healthcare policy. AI presents a transformative opportunity to enhance traditional HTA methodologies by significantly improving their accuracy and efficiency. It addresses long-standing limitations such as data gaps and time-intensive processes through automation, real-time data integration, and advanced predictive modeling, leading to faster and more informed decisions.
AI also plays a vital role in supporting personalized medicine and integrating real-world evidence (RWE). By analyzing large datasets from Electronic Health Records (EHRs), patient registries, and genomics, AI can refine the evaluation of individualized treatments and generate robust RWE, which is increasingly critical for guiding value-based pricing and reimbursement decisions. Furthermore, AI-driven Natural Language Processing (NLP) can automate and enhance systematic reviews, a core component of HTA, by efficiently extracting and synthesizing information from vast amounts of literature. AI also improves survival analysis, a critical component in HTA for predicting long-term drug benefits, especially in oncology and chronic diseases, by handling time-dependent data through advanced neural networks.
HTA frameworks, such as the EUnetHTA Core Model, are actively being adapted specifically for AI-based health technologies, defining key indicators and assessment topics relevant to these novel tools. Early HTA can provide an initial assessment of the potential health outcomes and cost-effectiveness of AI tools even at nascent stages of development.
A significant challenge in the evaluation of AI in healthcare is the gap between technical performance and real-world clinical impact. For instance, some analyses indicate that many AI systems lack rigorous scientific validation and demonstrate limited clinical impact beyond diagnostic accuracy. This is starkly illustrated by the RAPIDx AI trial, where the AI tool, despite its technical sophistication in identifying cardiac conditions, did not improve the primary composite clinical outcome of CV death, new/recurrent MI, and CV readmission within 6 months. This suggests that achieving high diagnostic accuracy, which is primarily a technical metric, does not automatically translate to improved patient outcomes in complex clinical environments. The implication is that the evaluation of AI in healthcare must evolve beyond solely technical performance metrics (e.g., sensitivity, specificity, AUC) to prioritize robust clinical trials that assess real-world patient outcomes. This necessitates a shift in research priorities and regulatory expectations, emphasizing effectiveness studies over mere efficacy. The inherent "black box" nature of some AI systems and the risk of "calibration drift" where performance degrades over time further complicate this, as initial performance may not be sustained, demanding continuous monitoring and re-validation to ensure sustained clinical impact and patient safety.
This leads to an evolving understanding of the role of Real-World Evidence (RWE) and Health Technology Assessment (HTA) in AI evaluation. HTA is crucial for informing policy and resource allocation decisions , and AI can significantly enhance HTA by integrating RWE from diverse sources like EHRs and wearables. AI models are also noted to continuously learn from real-world feedback, improving performance and reducing bias over time. This indicates a move beyond traditional, often slow, randomized controlled trials (RCTs) as the exclusive gold standard for evaluation. The rapid pace of AI innovation in healthcare demands agile and continuous evaluation methodologies that can keep pace. Traditional, lengthy RCTs may not be sufficient on their own. HTA frameworks, augmented by AI's capacity to process and learn from vast RWE, will become increasingly vital for dynamic assessment of AI's value, cost-effectiveness, and long-term impact across diverse patient populations. This necessitates the development of robust data governance, interoperability standards, and ethical guidelines for RWE collection and AI-driven HTA to ensure reliable, equitable, and timely assessments.
4. Demonstrated Impacts of AI Triage on Patient Outcomes and Operational Efficiency
Empirical evidence highlights the multifaceted impacts of AI triage, encompassing both direct clinical outcomes and significant operational improvements within healthcare settings.
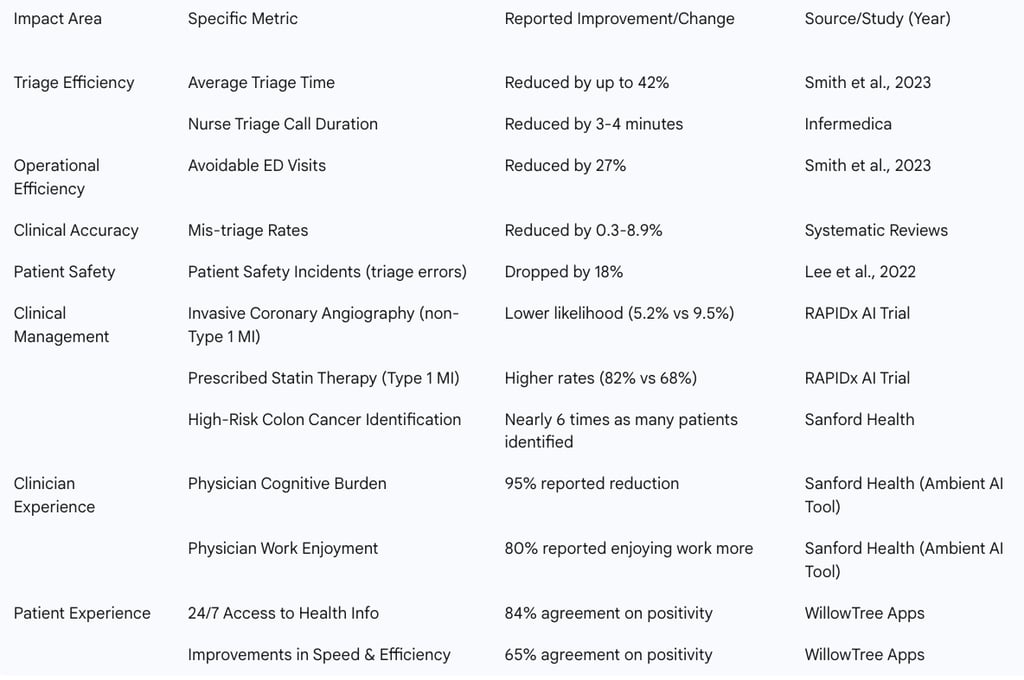
4.1. Evidence of Improved Triage Accuracy and Reduced Mis-Triage Rates
AI possesses the potential to significantly enhance the accuracy of triage assessments, leading to more appropriate patient prioritization and care pathways. Systematic reviews indicate that the application of machine learning algorithms has resulted in a reduction of mis-triage rates by 0.3-8.9%. This improvement is crucial, as accurate triage ensures that patients receive the appropriate level of care without unnecessary delays or over-utilization of resources. AI has also demonstrated superior performance compared to conventional triage methods in predicting patient outcomes more accurately , thereby enabling more precise and timely interventions. The use of AI has been particularly effective in identifying critical outcomes, such as the immediate need for care, which directly contributes to improved patient classification and reduces the risk of adverse events.
4.2. Impact on Patient Flow, Waiting Times, and Resource Optimization
One of the most consistently reported benefits of AI triage is its profound impact on operational efficiencies. AI systems can substantially reduce waiting times, efficiently allocate resources, and optimize patient flow within emergency departments. These AI-powered solutions streamline patient intake processes, effectively reduce bottlenecks in the ED, and accelerate the overall time-to-treatment for patients.
Quantifiable evidence supports these claims: a 2023 Journal of Medical Internet Research meta-analysis found that AI triage tools reduced avoidable ED visits by 27% and decreased the average triage time by an impressive 42%. AI significantly improves response time and minimizes the margin of error in patient classification, especially crucial in high-demand situations where rapid, accurate decisions are paramount. During the unprecedented challenges of the COVID-19 pandemic, AI proved essential in the remote triage of high-risk patients, ensuring the efficient utilization of resources in severely overcrowded settings. Beyond individual patient interactions, AI has shown effectiveness in predicting demand and managing resources efficiently, leading to improved overall clinical and operational outcomes. Furthermore, AI-backed tools have demonstrated greater accuracy than traditional methods in prioritizing patients during peak demand, ensuring that critical cases are identified and addressed promptly.
Innovative applications, such as pre-triage voice agents leveraging Neuro-Symbolic AI, have shown the ability to shorten nurse triage call durations by 3-4 minutes by efficiently gathering preliminary patient symptom information. These voice agents also contribute to smarter triage by prioritizing calls based on clinical urgency, enabling nurses to promptly address critical cases. AI-powered pre-visit triaging also holds the potential to reduce ED overcrowding and decrease overall patient wait times before arrival.
4.3. Effects on Specific Clinical Management Pathways and Patient Safety Incidents
Beyond general efficiency, AI triage has demonstrated specific impacts on clinical management and patient safety. Patient safety incidents directly related to triage errors have reportedly dropped by 18%.
The RAPIDx AI Trial provides a nuanced perspective on AI's clinical impact. This cluster-randomized trial investigated an AI tool for ED triage of suspected cardiac conditions. The primary endpoint, a composite of cardiovascular (CV) death, new/recurrent myocardial infarction (MI), and CV readmission within 6 months, was nearly identical between the AI-informed and control groups (26.0% vs 26.4%). The safety endpoint of all-cause death or MI within 30 days among those directly discharged from the ED was noninferior for AI-equipped hospitals (0.86% vs 1.1%; P for noninferiority < 0.001). While the overall composite outcome was not significantly improved, the AI tool did demonstrate clear benefits in tailoring management: for patients classified as not having type 1 MI (n=2,441), AI-informed care led to a lower likelihood of invasive coronary angiography (5.2% vs 9.5%), revascularization, and beta-blocker use. Conversely, for patients classified as having type 1 MI (n=578), those in the AI arm had higher rates of being prescribed statin therapy (82% vs 68%), P2Y12 inhibitor therapy (56% vs 44%), and mineralocorticoid receptor antagonists (26% vs 18%). An exploratory analysis, excluding STEMI patients (whose management is primarily ECG-guided), found a significant difference in CV death/MI favoring intervention hospitals (HR 0.81; 95% CI 0.66-0.99). This trial highlights the complexity of demonstrating direct, broad clinical outcome improvements, even when AI provides valuable decision support.
This demonstrates a nuanced reality of AI's clinical impact, distinguishing between direct and indirect benefits. While many sources broadly claim "improved patient outcomes" , the specific findings of the RAPIDx AI trial provide crucial detail. It showed no improvement in a broad composite clinical endpoint, yet demonstrated clear benefits in optimizing clinical pathways and tailoring management, such as reducing unnecessary procedures and increasing appropriate medication prescriptions. This suggests that AI's impact might be more indirect, enabling better decisions and resource utilization, which then should lead to improved outcomes, but these outcomes are multifactorial and harder to isolate. Quantifying AI's impact therefore requires highly specific and carefully chosen endpoints that reflect the direct effects of AI on decision-making and care processes. Focusing solely on broad, ultimate clinical outcomes may obscure the real value AI delivers in optimizing clinical pathways, reducing inappropriate interventions, and improving the efficiency of care delivery. This also underscores the need for longer-term studies and a deeper understanding of the complex causal chain from AI intervention to ultimate patient benefit.
Beyond cardiac care, AI has improved diagnostic investigation and optimized the triage of critically ill patients across various conditions. The technology has also facilitated the automation of routine tasks, freeing up healthcare professionals to focus on more complex, patient-centered care. Furthermore, AI has demonstrated capabilities in predicting clinical deterioration, enabling preventive interventions before conditions escalate.
Sanford Health's AI for Colon Cancer Screenings offers another compelling example. By developing an AI-driven risk score based on electronic health record (EHR) data, Sanford Health identified nearly six times as many patients at high risk of colon cancer. This significantly reduced an 18-month backlog for colonoscopies in some areas, leading to higher-risk patients being seen by gastroenterology specialists sooner, thereby improving access to critical preventative care.
4.4. Improvements in Patient and Clinician Experience
The impact of AI triage extends beyond clinical and operational metrics to significantly influence the experience of both patients and healthcare professionals. AI-powered patient triage systems directly contribute to higher patient satisfaction. Patients express considerable positivity towards AI in healthcare for several reasons, including 24/7 access to health information (84% agreement), the potential for holistic health insights (72%), expanded access to healthcare in underserved communities (68%), and improvements in speed and efficiency (65%).
For clinicians, AI can improve documentation accuracy and enhance decision support. The automation of routine tasks by AI optimizes time for healthcare professionals, allowing them to focus on more complex care and direct patient interaction.
Sanford Health's Ambient AI Listening Tool provides a compelling case study for improving clinician experience. A pilot program with 100 doctors demonstrated overwhelmingly positive results: 95% reported a reduction in cognitive burden, 88% would recommend the tool to partners, and four out of five (80%) reported enjoying their work more than before using the tool. This tool, which functioned as a scribe, allowed physicians to concentrate more on patient conversations and less on typing. This led to improved work-life balance for physicians, with one doctor noting he could finish charting earlier and participate in family activities before dinner. Critically, this improvement in physician experience simultaneously improved patient experience during appointments, aligning with the long-standing goals of both doctors and patients in healthcare.
AI voice agents further contribute to this by ensuring accurate and complete information collection, simplifying documentation, and facilitating smoother integration into electronic health records (EHRs).
This demonstrates AI's dual role in addressing healthcare burnout and patient dissatisfaction. AI's capacity to reduce physician cognitive burden and automate routine tasks concurrently addresses significant patient pain points such as information gaps, lack of 24/7 access, and long wait times. This dual benefit positions AI as a strategic solution for improving the overall healthcare ecosystem, tackling both provider well-being and patient satisfaction, which are often treated as separate challenges. AI triage is therefore not merely a technological upgrade for efficiency; it is a transformative tool that can simultaneously alleviate the immense pressures on healthcare professionals and significantly enhance the patient journey. This broader impact on "joy in work" for clinicians and "patient satisfaction" can lead to improved staff retention, reduced burnout, and increased patient loyalty—all substantial, albeit often harder to quantify, benefits for healthcare organizations. Therefore, the return on investment (ROI) of AI should encompass these critical human-centric benefits, not just traditional clinical or financial metrics.
Table 2: Summary of Quantified Impacts of AI Triage from Key Studies
Challenges and Limitations in AI Triage Implementation and Quantification
Despite the demonstrated benefits, the widespread and effective implementation and accurate quantification of AI triage systems face significant hurdles and inherent limitations.
5.1. Methodological Heterogeneity and Generalizability Issues in Current Research
A pervasive challenge in the evaluation of AI triage systems is the significant methodological heterogeneity observed across studies. This variability encompasses differences in study design, the characteristics of patient populations, the specific AI algorithms employed, and the outcome measures selected for evaluation. Such diversity makes direct comparisons between studies and the conduct of robust meta-analyses inherently challenging.
A notable limitation is the predominance of single-center studies in the current literature. Findings from these studies often have limited generalizability, as AI models developed and validated within a specific institutional context may not perform reliably when deployed in different geographic regions, healthcare systems with varying patient demographics, or diverse clinical settings. The concept of "universal generalizability" for AI algorithms in medicine is widely considered a myth for current AI technology , emphasizing the critical need for explicit eligibility criteria and precise specification of the real-world clinical setups where AI is intended for use during external testing. This underscores a clear call for rigorous multi-center validation and standardized outcome reporting to enhance the robustness, comparability, and broad applicability of research findings in this field.
5.2. Technical Challenges: Algorithmic Bias, Model Interpretability ("Black Box"), and Performance Degradation
Technical complexities present substantial barriers to the equitable and reliable deployment of AI triage.
Algorithmic Bias: AI systems are trained on vast datasets, and if these datasets reflect existing societal biases—such as historical disparities in healthcare access, quality of care, or outcomes for certain demographic groups—these biases can become ingrained in the AI algorithms themselves. This can lead to the perpetuation and amplification of unfair or discriminatory outcomes, particularly in critical areas like resource allocation and patient care. For example, if training data disproportionately represents certain demographics or lacks sufficient data for others, the AI could potentially misdiagnose or recommend less effective treatments for underrepresented groups, thereby exacerbating existing health inequities. Algorithmic bias is explicitly identified as a significant barrier to the widespread and equitable adoption of AI-driven triage. Ensuring inclusiveness and equity throughout both the design and usage phases of AI development is paramount to effectively combat these implicit biases.
Model Interpretability ("Black Box" Problem): Many AI systems, particularly complex machine learning models, operate as "black boxes," meaning their internal logic and the precise reasoning behind their outputs are not easily understood by users or affected parties. This lack of transparency can lead to doubt and mistrust among physicians, who are ultimately responsible for patient outcomes. Transparency and comprehensibility are highly desired for the effective control, monitoring, and correction of AI systems, especially in high-stakes clinical environments. The development of Explainable AI (XAI) is critical to address this challenge, as it aims to provide rationales or explanations to support user understanding of the model's operation, thereby enhancing trust and facilitating clinical decision-making.
Performance Degradation (Calibration Drift): A critical, often overlooked, challenge is that AI systems may experience performance degradation over time in real-world settings. This phenomenon, known as "calibration drift," occurs due to various factors such as shifting data distributions (e.g., changes in disease prevalence), evolving patient characteristics, updates to clinical protocols, and variations in data quality. When calibration drifts, a model's predicted probabilities may no longer accurately match actual outcomes, even if its ability to rank individuals by risk remains stable. This can lead to systematic overestimation or underestimation of risk, compromising the reliability of risk estimates and potentially resulting in suboptimal or inequitable clinical decisions. Such degradation is particularly critical in high-stakes tasks like risk stratification, triage, and prognostication, where miscalibrated predictions can misguide clinical decisions and erode trust.
5.3. Operational and Human Factors: Clinician Trust, Acceptance, Workflow Integration, and Potential Over-Reliance
Beyond technical issues, the successful implementation of AI triage is heavily influenced by operational and human factors. A recurring challenge is the insufficient metrics and evidence regarding clinician acceptance of AI systems. There can be inherent resistance from healthcare professionals to integrate AI into their established and often deeply ingrained workflows.
Practical workflow integration barriers are a significant concern, as AI tools must be seamlessly incorporated into existing clinical processes to avoid disruption, inefficiency, and increased burden on staff. Furthermore, concerns exist regarding the potential for over-reliance on automated decision-making in high-stakes clinical environments. While AI provides valuable assistance, it is universally acknowledged that it should always be used in conjunction with human expertise, with healthcare professionals exercising their clinical judgment when making final decisions about patient care. Patient sentiment also reflects concerns about human oversight of AI decisions , indicating that trust in AI extends beyond clinicians to the patient population itself.
The interplay of technical limitations and human factors significantly impacts adoption. The "black box" problem, where AI's decision-making logic is opaque , directly affects clinician trust and acceptance. If clinicians cannot understand the reasoning behind an AI's recommendation, they are less likely to integrate it into their workflow or trust its outputs, leading to "insufficient clinician acceptance". Similarly, algorithmic bias can lead to inequitable outcomes, further eroding trust and hindering widespread, ethical adoption. This creates a feedback loop where technical limitations exacerbate human resistance. Therefore, technical advancements in AI, such as developing explainable AI or mitigating bias, are necessary but not sufficient for successful implementation. They must be coupled with comprehensive strategies that address the human element: fostering trust through transparency, providing adequate training, and designing AI tools that genuinely augment and simplify, rather than complicate, clinical workflows. Failure to address the "black box" issue and build trust could perpetuate low adoption rates, limiting the collection of real-world data needed for further validation and improvement.
This leads to an understanding of the dynamic nature of AI performance in real-world healthcare. The concept of "calibration drift" is a critical, often overlooked, challenge. AI models, once deployed, are not static; their performance can degrade over time due to shifts in patient populations, disease prevalence, or evolving clinical protocols. This means an AI system performing well at initial deployment might become less reliable or even unsafe over months or years, posing significant safety concerns. The implication is that AI in healthcare cannot be treated as a "set it and forget it" solution. It necessitates continuous monitoring, re-calibration, and adaptive learning mechanisms to maintain performance, ensure patient safety, and sustain clinical utility. This has profound implications for the infrastructure, governance, and regulatory frameworks required to support AI in healthcare, moving from a one-time approval process to ongoing oversight and validation throughout the AI system's lifecycle. Healthcare organizations must also invest in data science capabilities for internal AI model maintenance and auditing.
Ethical and Regulatory Considerations for AI Triage
The deployment of AI in healthcare triage necessitates careful consideration of critical ethical dilemmas and navigation of an evolving regulatory landscape to ensure responsible innovation.
6.1. Addressing Bias and Discrimination in AI Algorithms
AI systems, by learning from vast datasets, unavoidably embed societal biases present in that data. This can lead to the perpetuation and amplification of unfair or discriminatory outcomes in crucial areas like resource allocation and patient care. For instance, if training data disproportionately represents certain demographics or lacks sufficient data for others, the AI could potentially misdiagnose or recommend less effective treatments for underrepresented groups, thereby exacerbating existing health inequities. Algorithmic bias is explicitly identified as a significant barrier to widespread adoption of AI-driven triage. Ensuring inclusiveness and equity in both the design and usage of AI is paramount to combat these implicit biases. Future development must prioritize robust ethical frameworks to ensure safe and equitable implementation.
6.2. Ensuring Transparency and Accountability in AI-Driven Decisions
The "black box" nature of many AI systems, where their internal workings and decision-making logic are opaque, poses a significant challenge. In critical domains like healthcare, transparency is vital to understand how decisions are made and to assign responsibility when errors or harm occur. Explainable AI (XAI) is being developed to address these challenges, aiming to characterize the model's fairness, accuracy, and potential bias by providing rationales or explanations for its outputs. Crucially, clinicians remain responsible for the medical decisions they make, even when supported by AI-enabled clinical decision support systems. This underscores the need for AI to be a decision support tool, not a replacement for human judgment. Patient concerns about human oversight of AI decisions further emphasize the need for clear accountability and interpretability.
6.3. Data Privacy, Security, and Surveillance Concerns
The effectiveness of AI often hinges on the availability and processing of large volumes of personal data. This raises significant concerns regarding how this sensitive patient information is collected, stored, and utilized. In healthcare, where patient health information is highly sensitive, preserving individuals' privacy and human rights is paramount. This necessitates robust safeguards against data breaches, unauthorized access to sensitive information, and protections from extensive surveillance. Compliance with regulations like GDPR (General Data Protection Regulation) is also a critical factor.
6.4. The Evolving Regulatory Landscape for AI in Healthcare
The number of AI-enabled medical devices listed by the United States Food and Drug Administration (FDA) has rapidly grown to over 1,000, indicating accelerating adoption. However, there is a recognized "lack of regulatory standards" and a clear need for "regulatory evolution" to keep pace with AI advancements. Health Technology Assessment (HTA) frameworks, which vary by country (e.g., NICE in the UK, ICER in the US, EUnetHTA in the EU), are crucial for informing policy decisions. AI can enhance these decision-making processes, but the frameworks themselves must adapt to AI's unique characteristics. The AI-Mind project, for instance, has developed an HTA framework specifically for AI-based health technologies, adapted from the EUnetHTA Core Model, demonstrating a proactive approach to regulatory adaptation.
A significant challenge is the inherent tension between data-driven AI and ethical principles. AI's power is derived from its ability to process vast datasets. However, these datasets are often repositories of historical biases and inherently contain sensitive personal information, raising significant privacy concerns. This creates a fundamental tension: the drive for data-driven precision in AI triage directly conflicts with the imperative to protect patient privacy and ensure equitable care, especially for vulnerable populations who might be underrepresented or misrepresented in training data. The implication is that ethical considerations are not merely add-ons but fundamental constraints that must guide AI development and deployment in healthcare. Achieving "equitable implementation" requires proactive measures to mitigate bias at every stage of the AI lifecycle, from data collection and model training to deployment and continuous monitoring. This necessitates a robust legal and ethical framework that balances innovation with patient rights and societal fairness, potentially leading to more stringent approval processes and a slower, more deliberate adoption pace than in other industries.
This also highlights the issue of regulatory lag and the need for adaptive governance. The rapid increase in FDA-approved AI medical devices contrasts with the acknowledged "lack of regulatory standards" and the call for "regulatory evolution". This indicates that AI innovation is outpacing the development of comprehensive regulatory frameworks. Furthermore, the "black box" nature of AI and the potential for "calibration drift" challenge traditional, static regulatory approval processes. The implication is that current regulatory models, often designed for static medical devices or pharmaceuticals, are often ill-suited for dynamic, continuously learning AI systems. There is an urgent need for adaptive, iterative regulatory frameworks that can ensure ongoing safety, efficacy, and ethical compliance throughout an AI system's lifecycle. This might involve "living" approvals, robust post-market surveillance for performance degradation, and international collaboration to standardize HTA and regulatory approaches for AI in healthcare to facilitate responsible global adoption.
Future Directions and Recommendations
The trajectory of AI in healthcare triage points towards a future where its transformative potential can be fully realized, provided strategic imperatives in research, implementation, and policy are addressed.
7.1. Call for Rigorous Multi-Center Validation and Standardized Outcome Reporting
To overcome the limitations of methodological heterogeneity and the predominance of single-center studies, AI-based triage systems require rigorous multi-center validation. This will significantly enhance the generalizability and reliability of findings across diverse patient populations and varied healthcare settings, moving beyond isolated successes. Furthermore, standardized outcome reporting is crucial to enable meaningful comparisons across different studies and to facilitate future meta-analyses. This standardization can also help unify Health Technology Assessment (HTA) methodologies across different countries, making assessments more comparable and scalable, which is vital for global adoption and policy coherence.
7.2. Prioritizing Explainable AI, Robust Ethical Frameworks, and Continuous Clinician Engagement
Future development efforts must prioritize the creation of inherently explainable algorithms to enhance trust and facilitate clinical decision-making. Explainable AI is essential not only for justifying AI outputs and enabling human oversight but also for potentially discovering novel clinical insights by revealing unexpected correlations or contributing factors. The development and strict adherence to robust ethical frameworks are paramount to ensure the safe, fair, and equitable implementation of AI triage, proactively addressing concerns such as bias, discrimination, and privacy. Continuous clinician engagement is vital for successful adoption and integration. AI should be designed to support, not replace, the human touch, fostering a collaborative environment where healthcare professionals remain central to patient care. Addressing clinician acceptance and workflow integration barriers is a key step in ensuring that AI tools are embraced and effectively utilized.
7.3. Potential for Integration with Emerging Technologies and Personalized Medicine
The future of AI triage lies in its deeper and more seamless integration with emerging technologies. This includes the incorporation of wearable sensors and advanced digital diagnostics, which will enable continuous, real-time triage for high-risk populations and support proactive interventions before conditions escalate. AI will increasingly tailor triage recommendations based on individual patient risk profiles, social determinants of health, and comprehensive longitudinal health records, moving towards truly personalized medicine. This evolution aligns with the concept of personalized value assessments in HTA, ensuring that pricing models for treatments are fair and aligned with individual patient needs and treatment efficacy. AI's unique ability to combine data from traditional clinical trials with vast real-world evidence, including electronic health records (EHRs) and genomics, will further improve the accuracy and predictive power of patient outcome predictions. Seamless integration with telemedicine workflows and robust EHR interoperability will be critical enablers for this advanced, interconnected future of AI-powered care.
7.4. Strategic Recommendations for Stakeholders
The path forward for AI triage requires concerted effort from all stakeholders.
For AI Developers: Focus on building inherently explainable and bias-mitigated AI algorithms. Prioritize human-centered design to ensure seamless workflow integration and foster effective human-AI collaboration. This means moving beyond mere technical accuracy to consider the usability and trustworthiness of the system in a clinical context.
For Healthcare Organizations: Invest in robust data infrastructure and governance frameworks to ensure data quality, privacy, and security, which are foundational for reliable AI. Implement pilot programs to test and refine AI solutions in real-world settings, allowing for iterative improvements before widespread deployment. Prioritize comprehensive clinician training and proactive change management strategies to foster trust and acceptance, recognizing that technology adoption is as much about human factors as it is about technical capability. Establish mechanisms for continuous monitoring of AI performance degradation and recalibration to ensure sustained accuracy and safety over time.
For Policymakers and Regulators: Develop adaptive and iterative regulatory frameworks that can keep pace with dynamic AI systems, potentially including "living" approvals and robust post-market surveillance, moving beyond static approval processes. Promote and fund multi-center validation studies and initiatives for standardized outcome reporting to build a stronger evidence base. Support research into long-term and patient-centered outcomes, as well as critical equity considerations in AI deployment, ensuring benefits are equitably distributed.
For Researchers: Prioritize prospective, multi-center studies with standardized methodologies and outcome measures to enhance generalizability. Focus on quantifying long-term and patient-centered outcomes, moving beyond efficiency metrics to capture the full spectrum of AI's impact on patient well-being. Develop and validate methodologies for robust real-world evidence integration and advanced Health Technology Assessment for AI, which are crucial for dynamic and continuous evaluation.
The imperative for a "learning healthcare system" driven by AI is clear. The continuous need for monitoring AI performance , ongoing learning from real-world feedback , and dynamic HTA models collectively point towards a fundamental transformation of healthcare into a system that constantly learns and adapts. This implies a shift from static AI deployments to a continuous cycle of data collection, AI refinement, and outcome measurement. The future of AI in healthcare triage is not merely about deploying smart tools, but about fundamentally transforming healthcare into a "learning healthcare system." In this paradigm, data generated from AI-powered interventions continuously informs and improves clinical practice, resource allocation, and policy. This requires significant, sustained investment in advanced data infrastructure, sophisticated analytical capabilities, and a cultural shift towards continuous improvement and adaptation within healthcare organizations and regulatory bodies.
Finally, bridging the "last mile" of AI adoption—trust, training, and integration—is paramount. Despite the clear operational and some clinical benefits, challenges such as "insufficient clinician acceptance" and "workflow integration barriers" persist. The RAPIDx AI trial's modest impact on broad outcomes implicitly suggests that even a technically well-designed AI tool might not achieve its full potential if clinicians do not fully engage with its insights. This indicates that technological sophistication alone is insufficient; human factors represent the critical "last mile" for successful adoption. The ultimate success and widespread impact of AI triage hinge not just on algorithmic accuracy but equally on effective human-centered design, comprehensive training programs, and thoughtful integration into existing clinical workflows. Future efforts must prioritize co-creation with end-users (clinicians and patients) to build trust, address practical pain points, and ensure that AI tools are perceived as valuable, intuitive assistants rather than disruptive replacements. This means that implementation science, human factors engineering, and change management strategies will be as critical as AI development itself in realizing the full potential of AI triage.
FAQ Section
What is AI triage in healthcare?
AI triage in healthcare refers to the use of artificial intelligence algorithms to help prioritize and direct patients to the most appropriate level of care based on their symptoms, medical history, and clinical presentation. These systems analyze multiple data points to predict acuity, risk, and resource needs more accurately than traditional triage methods.
How does AI triage improve patient outcomes?
AI triage improves patient outcomes by reducing wait times for critical cases, increasing diagnostic accuracy, enabling earlier intervention for time-sensitive conditions, optimizing resource allocation, and identifying subtle risk patterns that might be missed by traditional triage approaches. Research from 2025 shows significant reductions in mortality, complications, and hospital length of stay following AI triage implementation.
What types of healthcare facilities can benefit from AI triage?
All types of healthcare facilities can benefit from AI triage, including emergency departments, primary care practices, urgent care centers, specialty clinics, rural hospitals, and telehealth services. The technology can be scaled and adapted to different clinical contexts, with research showing significant improvements across diverse healthcare settings.
Is AI triage meant to replace healthcare professionals?
No, AI triage is designed to augment rather than replace healthcare professionals. The most successful implementations position AI as a decision support tool that helps clinicians make more informed and efficient decisions while allowing them to focus more attention on complex cases and human aspects of care that require professional judgment and empathy.
What data is used to train AI triage systems?
AI triage systems are typically trained on diverse data sources including electronic health records, vital signs, laboratory results, imaging studies, clinician notes, patient-reported symptoms, and historical outcome data. Advanced systems may incorporate social determinants of health, genomic data, and population health statistics to provide more comprehensive risk assessment.
How accurate are current AI triage systems?
The most advanced AI triage systems achieve overall accuracy rates exceeding 90% across a broad range of clinical presentations, with particularly high performance in identifying high-risk conditions. Research from 2025 shows these systems consistently outperform traditional triage protocols and match or exceed the accuracy of experienced clinicians, especially for complex or atypical presentations.
What challenges exist in implementing AI triage?
Key implementation challenges include integration with existing electronic health records, staff training and acceptance, workflow redesign, addressing potential algorithmic bias, ensuring appropriate oversight, maintaining privacy and security, and managing the transition period. Successful implementations address these challenges through careful planning, stakeholder engagement, and phased approaches.
How does AI triage impact healthcare equity?
When properly designed and implemented, AI triage can help reduce healthcare disparities by standardizing initial assessment processes, reducing implicit bias in prioritization decisions, and helping identify high-risk patients regardless of their ability to advocate for themselves. However, ongoing monitoring and bias mitigation strategies are essential to ensure these systems don't inadvertently perpetuate existing inequities.
What ROI can healthcare facilities expect from AI triage implementation?
Healthcare facilities implementing AI triage typically report positive return on investment within 12-18 months, driven by improved operational efficiency, reduced unnecessary testing, decreased liability exposure from missed diagnoses, shorter lengths of stay, improved resource utilization, and better patient outcomes. Studies from 2025 report average ROI ratios between 3:1 and 5:1 over a three-year period.
How is AI triage likely to evolve in the future?
Future AI triage evolution will likely include more multimodal sensing capabilities, continuous rather than episodic risk assessment, deeper integration with precision medicine, greater incorporation of social determinants of health, expanded patient-facing applications, and more sophisticated predictive modeling of likely clinical trajectories to enable increasingly personalized and proactive care planning.
Additional Resources
National Consortium on AI in Healthcare: 2025 Best Practice Guidelines for AI Triage Implementation
Journal of Emergency Medicine: Special Issue on AI Triage Outcomes (March 2025)
Healthcare Equity Initiative: Ensuring Algorithmic Fairness in Clinical Decision Support
American College of Emergency Physicians: Position Statement on AI Augmented Triage (January 2025)
Institute for Healthcare Improvement: Measuring and Optimizing AI Triage Impact
