Patient Empowerment Through Self-Triage Tools
Explore how digital self-triage tools are revolutionizing patient engagement while navigating clinical limitations, featuring insights on implementation strategies, risk management, and the future of consumer-directed healthcare navigation.


The landscape of healthcare is undergoing a profound transformation, driven significantly by the advent and increasing sophistication of self-triage tools. These digital solutions, encompassing symptom checkers, virtual triage systems, and online consultation platforms, are redefining the patient's role from passive recipient to active participant in their health journey. By enabling individuals to assess their symptoms, access reliable health information, and navigate care pathways independently, these tools foster a greater sense of autonomy and self-efficacy.
The widespread adoption of self-triage technologies offers multifaceted benefits across the healthcare ecosystem. Patients gain unprecedented 24/7 access to guidance, experience reduced anxiety, and are directed to the most appropriate care settings, thereby decreasing unnecessary emergency room visits and promoting self-care. For healthcare providers, these tools streamline workflows, reduce administrative burdens, and enhance patient safety by providing crucial pre-consultation data. At a systemic level, they contribute to significant cost savings, optimize resource allocation, and offer valuable population health insights, positioning data as a strategic asset for proactive health management.
However, the integration of self-triage tools is not without its challenges. Concerns persist regarding diagnostic and triage accuracy, particularly the tendency towards overtriage and the potential for undertriage in critical cases. The pervasive digital divide, characterized by disparities in digital literacy and broadband access, threatens to exacerbate existing health inequities if not proactively addressed through inclusive design and policy. Furthermore, issues of patient acceptance, trust, and the inherent inability of these tools to perform physical examinations necessitate careful consideration.
The future of self-triage is inextricably linked to advancements in Artificial Intelligence and predictive analytics. These technologies promise more personalized guidance, proactive health management, and seamless interoperability within broader digital health ecosystems. Realizing this potential, however, demands a concerted, interdisciplinary effort. Recommendations for stakeholders include prioritizing ethical guidelines, addressing algorithmic bias, ensuring seamless system integration, and fostering continuous education for both clinicians and patients. Adaptive regulatory frameworks are essential to keep pace with innovation while safeguarding patient safety and promoting equitable access. Ultimately, the successful evolution of self-triage tools hinges on building a virtuous cycle of trust, innovation, and patient-centered design, thereby truly revolutionizing healthcare access and outcomes.
1. Introduction: Defining Patient Empowerment and Self-Triage Tools
The modern healthcare paradigm is increasingly shifting towards a model that emphasizes individual agency and informed participation. This evolution is encapsulated by the concept of patient empowerment, a critical driver in the adoption of innovative digital health solutions, particularly self-triage tools.
1.1. Conceptualizing Patient Empowerment in Healthcare
Patient empowerment in healthcare signifies a fundamental shift, enabling individuals to assume a more active and informed role in managing their health and care decisions. This involves several key processes: robust information sharing, effective doctor-patient communication, collaborative shared decision-making, and proactive patient self-care.This approach provides patients with a greater sense of control over their health and overall well-being. Traditionally, patients have often been positioned as passive recipients of medical care, relying heavily on professional directives. However, the contemporary emphasis on "empowerment," "control," and "informed decisions" underscores a profound redefinition of this role. Self-triage tools are not merely instruments of efficiency; they are foundational mechanisms that facilitate this reorientation, transitioning patients from a reactive stance to an engaged partnership in their health journey. This transformative dynamic fundamentally alters the traditional patient-provider relationship, fostering a more collaborative and personalized care experience.
1.2. Definition and Evolution of Self-Triage Tools
Self-triage tools, frequently referred to as symptom-checkers or medical triage tools, are digital applications, accessible via websites, mobile applications, or patient portals, designed to enable individuals to assess their symptoms and health needs. Their core function is to guide users toward appropriate care options, discerning whether in-person medical attention is necessary or if symptoms can be effectively managed at home.
The adoption of these tools experienced a significant acceleration, particularly during the COVID-19 pandemic. This period necessitated innovative solutions to manage unprecedented patient surges and alleviate the immense burden on acute care services. The evolution of self-triage has progressed markedly from rudimentary manual triage processes. Initially, structured digital systems emerged, often built upon decision tree logic or standardized clinical protocols, such as the widely recognized Schmitt-Thompson protocols. More recently, Artificial Intelligence (AI) and Machine Learning (ML) have become pivotal, enabling sophisticated interpretation of patient-reported symptoms and the prediction of health issues based on advanced algorithms. This progression from traditional nurse call centers to rule-based and subsequently Large Language Model (LLM)-based virtual triage systems illustrates a continuous drive towards greater automation and intelligence. This rapid adoption and ongoing evolution, particularly highlighted by the demands of the pandemic, demonstrate that these tools are not simply technological novelties. Instead, they represent a systemic and strategic response to the escalating demands and inherent resource limitations within healthcare systems. The continuous progression from manual to structured digital, and then to AI-supported systems, reflects an enduring commitment to scale healthcare access and efficiency in the face of growing patient populations and persistent staff burnout, indicating a long-term strategic shift rather than a temporary measure.
2. Types and Functionalities of Digital Self-Triage Tools
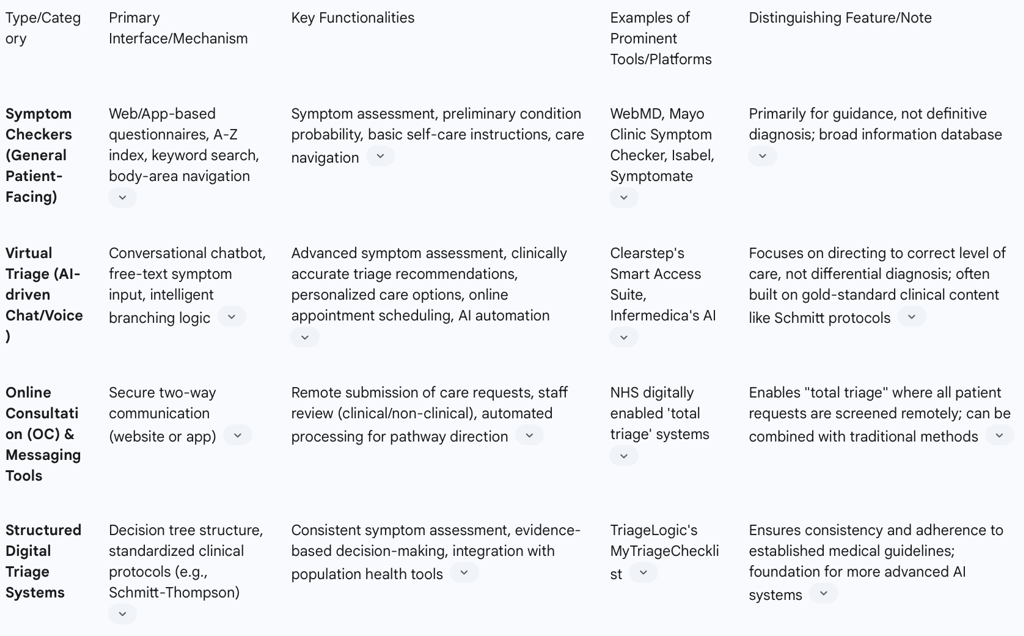
Digital self-triage tools encompass a diverse array of formats and functionalities, meticulously designed to meet varied patient needs and organizational requirements within the healthcare ecosystem.
2.1. Categorization of Self-Triage Tools
The landscape of self-triage tools can be broadly categorized based on their primary interface, underlying technology, and intended use:
Symptom Checkers (Patient-Facing): These are widely accessible online tools, typically websites or mobile applications, where users input their symptoms to receive potential diagnoses or, more commonly, triage recommendations. Prominent examples in the market include Docus AI, WebMD, Isabel, Ada, Mayo Clinic, Symptomate, and Buoy. It is crucial to note that their primary design is for triage, guiding patients to the appropriate level of care, rather than providing definitive diagnoses.
Online Consultation (OC) and Online Messaging (OM) Tools: Employed for remote triage, these tools facilitate patients in submitting their care requests digitally. The information provided is subsequently reviewed by either clinical or non-clinical staff, or it can be automatically processed by the online consultation platform itself. The objective is to direct patients to the most relevant consultation type, service, or self-directed care pathway.Comprehensive triage systems, where all patient requests are remotely screened, frequently integrate both digital and traditional communication methods to achieve this.
Virtual Triage Systems: Often powered by Artificial Intelligence, these systems leverage chat or voice interfaces, allowing patients to input symptoms using free-text descriptions. They then ask a series of clinically relevant follow-up questions, mimicking the interaction with a human medical professional. These systems are designed to accurately route patients to the most clinically appropriate resources, provide personalized care options, and facilitate online appointment scheduling. Clearstep's Smart Access Suite is a notable example in this category, known for its evidence-based approach built on gold-standard clinical content.
Structured Digital Triage Systems: These tools are characterized by their integration of standardized clinical protocols, such as the widely recognized Schmitt-Thompson protocols. They systematically guide symptom assessment and decision-making, thereby ensuring consistency and evidence-based recommendations across patient interactions.
2.2. Core Functionalities and Features
The operational capabilities of these self-triage tools are extensive and continually evolving:
Symptom Assessment: Tools employ various interfaces for symptom evaluation, including simple decision tree structures , sophisticated conversational chatbots with intelligent branching logic , or structured checklist formats that present symptom scenarios in order of clinical severity. They meticulously collect detailed information encompassing physical symptoms, behavioral changes, symptom duration, progression, severity indicators, and any related complications.
Care Navigation and Signposting: A fundamental function is to accurately direct patients to the most appropriate level of care—be it emergency, urgent, routine, or self-care—and to relevant medical facilities or services. These care pathways can be highly customized to align with a healthcare organization's specific network and available resources.
Preliminary Diagnosis and Condition Probability: While explicitly stating they do not provide definitive diagnoses, these tools can offer preliminary diagnostic information, calculate the probability of certain conditions, or generate a list of possible conditions based on the user's input.
Self-Care Instructions: Many self-triage tools provide comprehensive, step-by-step self-care guidance. This often includes accurate over-the-counter medication dosage charts, illustrative first aid procedures, and resources for behavioral health concerns.
AI and Machine Learning Integration: Artificial Intelligence plays a pivotal role in enhancing the capabilities of these tools. AI algorithms interpret patient-reported symptoms, predict potential health issues, and automate initial assessments, thereby significantly improving both accuracy and operational efficiency. Advanced AI systems are capable of rapidly analyzing multiple symptoms and associated risk factors.
Integration with Existing Systems: Seamless integration with Electronic Health Records (EHRs) and patient portals is a critical feature, facilitating efficient data sharing, streamlined appointment scheduling, and ensuring continuity of care across different healthcare touchpoints.
Administrative Automation: These tools can automate routine patient inquiries, appointment scheduling, and various other administrative tasks. This automation significantly reduces the manual workload on healthcare staff, allowing them to focus on more complex patient care activities.
Customization and Branding: Many platforms offer extensive white-labeling and customization options, allowing healthcare organizations to align the tool's visual experience with their brand identity. This ensures a seamless and cohesive patient experience that reinforces the organization's presence.
Analytics and Reporting: Built-in dashboards and reporting functionalities track usage patterns, conversion metrics, and patient needs and preferences. This provides invaluable data for optimizing digital pathways to care delivery, improving resource distribution, and informing strategic planning.
Multilingual Support and Age Inclusivity: To enhance accessibility and equity, some tools offer multiple language options and support assessments for all age groups, including specialized pediatric protocols reviewed by organizations like the American Academy of Pediatrics.
The evolution from simple decision tree models and basic questionnaires to sophisticated AI-powered conversational interfaces and free-text input signifies a significant maturation in digital health interface design. This progression moves beyond mere data collection to more intuitive, human-like interactions, which can substantially enhance user engagement and the richness of collected symptom data, potentially leading to more accurate triage recommendations. Furthermore, the recurring emphasis on integration with existing systems, including EHRs and patient portals, is not simply a desirable feature but a critical strategic imperative. Without seamless interoperability, the full benefits of self-triage tools—such as continuity of care, reduced manual data entry, and comprehensive patient views—cannot be fully realized. This highlights that the value of these tools is maximized when they function as an integrated component of a broader digital health ecosystem, rather than as standalone applications.
Table 1: Key Types and Functionalities of Self-Triage Tools

3. Mechanisms of Patient Empowerment through Self-Triage
Self-triage tools contribute to patient empowerment by fundamentally shifting the locus of control and information access within the healthcare continuum. This reorientation enables individuals to become more proactive and informed participants in their own health management.
3.1. Enhancing Patient Autonomy and Self-Care Capabilities
Patients gain a significant sense of control over their health and overall well-being by actively engaging in the assessment of their symptoms and health needs. These digital tools empower individuals to independently determine the appropriate level of care, effectively distinguishing between situations that necessitate immediate in-person medical attention and those that can be safely and appropriately managed with self-care at home. This newfound autonomy reduces reliance on potentially confusing or unreliable information often found through general internet searches. Furthermore, the provision of detailed self-care instructions, which include guidance on over-the-counter medication dosages and illustrated first aid procedures, directly supports patients in confidently managing minor illnesses independently.
3.2. Improving Health Literacy and Access to Information
Self-triage tools are instrumental in providing patients with accurate and real-time recommendations regarding their health concerns. They offer thorough information on potential causes of symptoms and clearly outline suggested next steps for care. This immediate and direct access to reliable, evidence-based information plays a crucial role in enhancing health literacy. Users are able to learn about various medical conditions, build a clearer understanding of symptom progression, and become more actively engaged in their personal healthcare journey. The provision of immediate, structured, and clinically vetted information directly addresses the common patient dilemma of uncertainty about symptoms and appropriate care. This readily available and trustworthy information serves to reduce stress, anxiety, and worry, which are often significant psychological barriers to seeking timely and appropriate medical attention. This proactive provision of information empowers patients not just with factual knowledge, but also with increased confidence and peace of mind.
3.3. Facilitating Shared Decision-Making with Clinicians
Symptom checkers enable patients to systematically gather and organize their medical data before a consultation, which can then be seamlessly shared with their healthcare providers. This pre-visit information allows clinicians to gain valuable insights into the patient's condition and history, significantly saving time during the actual consultation and fostering more meaningful and productive patient-doctor interactions. Research indicates that when individuals utilize high-performing Symptom-Assessment Applications (SAAs), their decision accuracy in self-triage can improve. While users may rely on the technology for information gathering and initial analysis, they ultimately retain the responsibility for integrating this information and making the final decision regarding their care. This dynamic supports a "human-in-the-loop" model of decision-making, where technology augments, rather than replaces, human judgment. The ability of self-triage tools to collect and present patient data prior to a consultation fundamentally alters the initial phase of patient-provider interaction. Instead of starting from a blank slate, clinicians can begin with a pre-analyzed summary of symptoms and concerns, thereby shifting the focus of the consultation from basic information gathering to deeper discussion, shared understanding, and truly collaborative decision-making. This represents a significant step towards a more efficient and humanized healthcare experience, where technology serves to facilitate, rather than diminish, meaningful clinical engagement.
4. Benefits for Patients, Providers, and Healthcare Systems
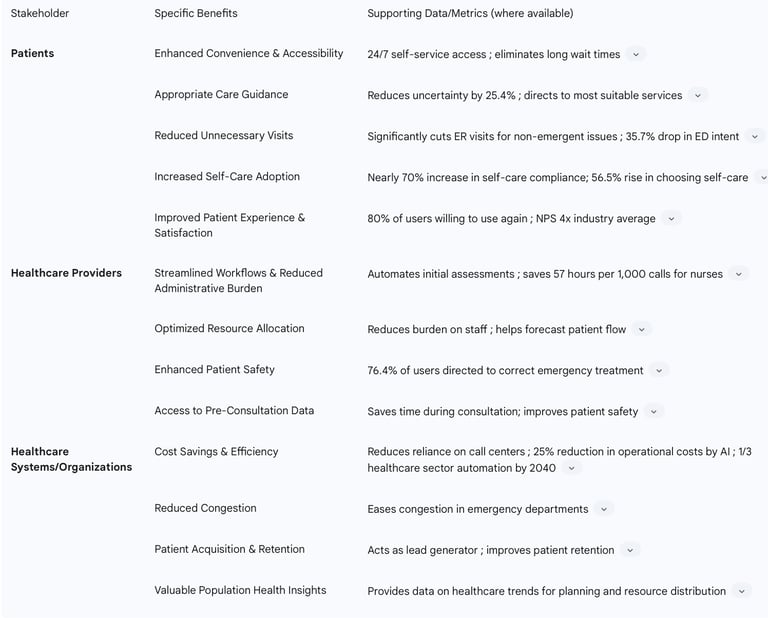
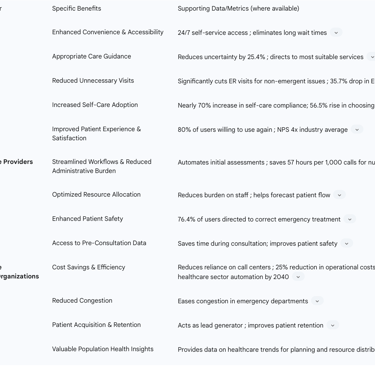
The widespread adoption and strategic implementation of self-triage tools yield substantial advantages across the entire healthcare ecosystem, benefiting individual patients, healthcare providers, and the broader healthcare system.
4.1. Benefits for Patients
Self-triage tools offer a multitude of direct benefits to patients, enhancing their experience and improving health outcomes:
Enhanced Convenience and Accessibility: Patients gain 24/7 self-service access to symptom assessments and comprehensive healthcare navigation support, effectively eliminating the long wait and handling times often associated with traditional care access points. These tools are designed for immediate availability and can be accessed conveniently via desktop computers or mobile devices.
Appropriate Care Guidance: These tools are highly effective in directing patients to the most suitable care services, whether it be an emergency department, urgent care, a general practitioner, or self-care at home. This precise guidance has been shown to reduce patient uncertainty about their care needs by an estimated 25.4%.
Reduced Unnecessary Visits: A significant advantage is the substantial reduction in unnecessary emergency room visits for non-emergent issues. Studies indicate a reported 35.7% drop in patients' intention to seek emergency care after using virtual triage tools.
Increased Self-Care Adoption: Patients are more inclined to follow self-care advice provided by these tools, with research demonstrating nearly a 70% increase in compliance with such recommendations and a 56.5% rise in individuals choosing self-care options.
Improved Patient Experience and Satisfaction: These tools contribute to a better overall patient experience, characterized by convenience, ease of use, and informative interactions. High satisfaction rates are consistently reported, with approximately 80% of users indicating a willingness to use them again. Some advanced tools even achieve a Net Promoter Score (NPS) four times the industry average, reflecting exceptional user satisfaction.
4.2. Benefits for Healthcare Providers
Healthcare providers experience significant operational and clinical advantages from the integration of self-triage tools:
Streamlined Workflows and Reduced Administrative Burden: Self-triage tools automate initial patient assessments, substantially decreasing the volume of manual tasks and data entry that frequently contribute to staff dissatisfaction and burnout. This automation frees up valuable time for healthcare professionals, allowing them to concentrate on more complex clinical cases and deliver higher-value patient care. For instance, automation can save nurses approximately 57 hours per 1,000 calls by handling repetitive work.
Optimized Resource Allocation: By efficiently directing patients to the correct care channels based on their symptoms, these tools reduce the overall burden on healthcare staff and provide data that helps forecast patient flow. This enables better organization and allocation of human resources, ensuring that staff are deployed where they are most needed.
Enhanced Patient Safety: For patients presenting with serious symptoms, virtual triage tools significantly improve the likelihood of making the correct urgent care choices. Data indicates that 76.4% of users who initially planned inappropriate care were accurately directed to the right emergency treatment after using a triage tool.
Access to Pre-Consultation Data: Clinicians gain valuable insights into a patient's symptoms and medical history even before the consultation begins. This pre-visit data collection not only saves time during the appointment but also enhances patient safety, particularly for individuals with complex medical histories who might otherwise forget critical details.
4.3. Benefits for Healthcare Systems and Organizations
At the organizational and systemic level, self-triage tools contribute to greater efficiency, financial sustainability, and improved public health management:
Cost Savings and Efficiency: These tools demonstrably reduce reliance on expensive call centers and significantly cut down the number of unnecessary emergency visits, leading to substantial cost savings. AI-driven predictive analytics, when integrated, can further reduce overall operational costs by approximately 25%. Projections suggest that over one-third of the healthcare sector's operations could be automated by 2040, underscoring the long-term potential for efficiency gains.
Reduced Congestion: By effectively diverting non-emergent cases to more appropriate care settings, self-triage tools play a crucial role in easing congestion in overcrowded emergency departments.
Patient Acquisition and Retention: Self-triage tools function as effective lead generators by identifying and guiding online consumers with care-seeking intent to book care within the organization, demonstrating a significant return on investment for current clients. They also contribute to improved patient retention by simplifying the next steps in care and fostering a positive ongoing relationship.
Valuable Population Health Insights: The comprehensive data collected through these tools—including symptom patterns, risk factors, and care-seeking behaviors—provides invaluable information about broader healthcare trends. This data enables better planning, more efficient resource distribution, and the development of highly targeted marketing campaigns for preventive medicine initiatives.
The consistent emphasis on financial benefits, such as reduced operational costs, decreased reliance on call centers, and fewer unnecessary emergency room visits, underscores a significant underlying economic imperative for healthcare organizations to invest in self-triage tools. This indicates that the widespread adoption of these technologies is not solely driven by altruistic motives but is also a strategic business decision aimed at optimizing resource utilization and improving financial performance. Beyond individual patient benefits, the capacity of self-triage tools to collect and analyze aggregated data on symptoms, risk factors, and care-seeking behaviors transforms this information into a strategic asset for healthcare systems. This data empowers proactive planning, informs resource distribution, and facilitates targeted public health interventions, signaling a definitive shift towards data-driven population health management and potentially real-time epidemiological surveillance.
Table 2: Benefits of Self-Triage Tools by Stakeholder
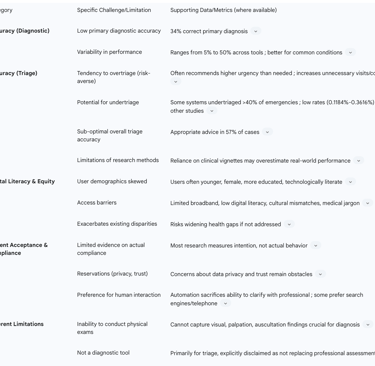
5. Challenges and Limitations: Accuracy, Equity, and Acceptance
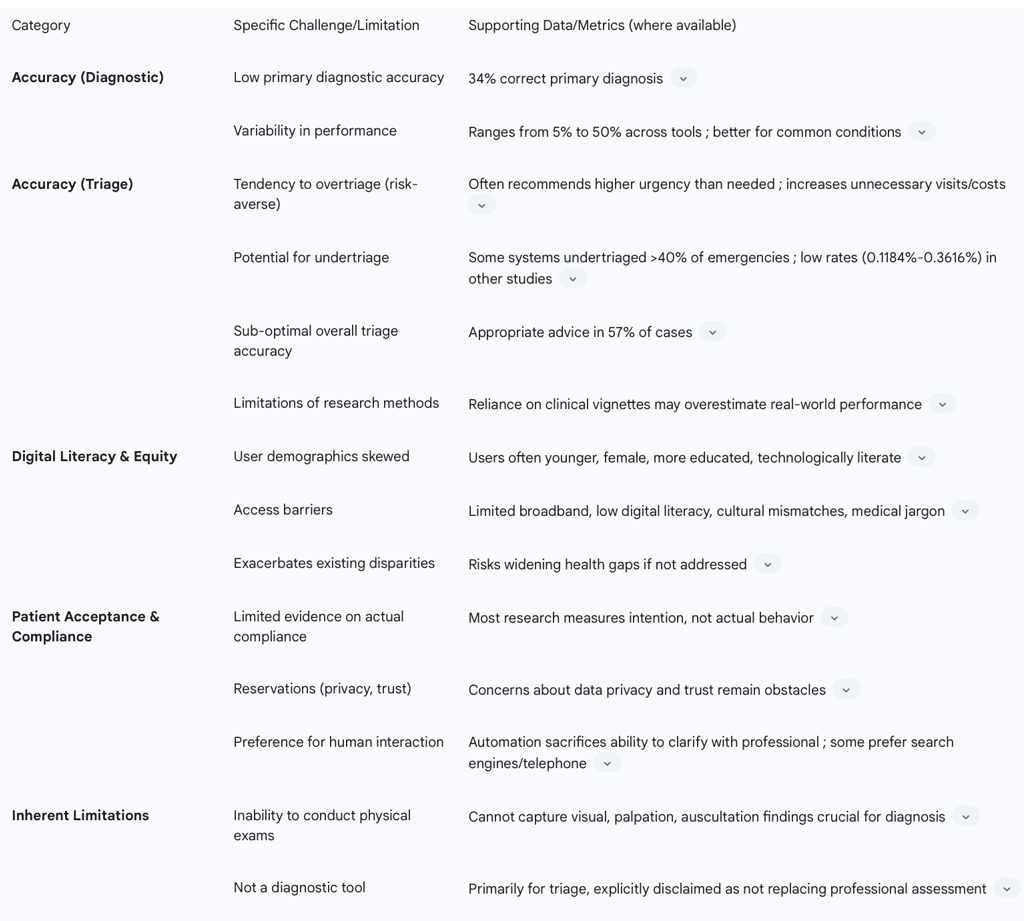
Despite the substantial benefits offered by self-triage tools, their safe, equitable, and effective integration into healthcare systems necessitates a thorough understanding and proactive addressing of inherent challenges and limitations.
5.1. Diagnostic and Triage Accuracy Concerns
The performance of self-triage tools in terms of diagnostic and triage accuracy remains a critical area of scrutiny. Studies consistently highlight limitations:
Overall Accuracy: Research indicates that self-triage tools have notable deficits in diagnostic accuracy. A landmark study from 2015 found that symptom checkers provided the correct primary diagnosis in only 34% of cases, and the correct diagnosis was listed within the top 20 suggestions in 58% of cases. Diagnostic accuracy exhibits significant variability across different platforms, user demographics, and specific diseases, generally performing more effectively for common conditions compared to rare diagnoses.
Triage Accuracy: While generally higher than diagnostic accuracy, appropriate triage advice is provided in approximately 57% of cases. Triage accuracy tends to be higher for emergent cases (around 80%) compared to non-emergent (55%) and self-care cases (33%). This disparity suggests that while tools are relatively good at identifying severe conditions, their guidance for less urgent or self-manageable issues is less reliable.
Risk-Averse Nature (Overtriage): Digital triage services are inherently designed to be risk-averse, prioritizing sensitivity over specificity. This often results in over-triaging, where a higher urgency level is recommended than is objectively necessary. Such caution, while seemingly safe, can lead to an increase in unnecessary visits to healthcare facilities and, consequently, higher healthcare costs for both individuals and the system.
Undertriage Risk: Conversely, there remains a risk of undertriage, where a serious condition is not identified as urgent. While some studies report very low rates of potentially hazardous undertriage (e.g., 0.1184% to 0.3616% in one large study) , other research has found that some systems undertriaged over 40% of emergencies, posing significant patient safety risks. This highlights a fundamental safety-efficiency paradox: optimizing self-triage tools requires a delicate balance, as being overly cautious burdens the system, while being too lenient risks patient harm. This indicates that improving accuracy is not a simple linear progression but a complex optimization problem with critical implications for patient outcomes and resource utilization.
Limitations of Research Methodologies: A substantial portion of studies evaluating accuracy rely on clinical vignettes, which are standardized patient scenarios. This methodology may overestimate real-world performance, as actual patients might struggle to describe their symptoms with the same precision or use varied terminology.Furthermore, there is often a lack of direct comparison with human clinicians using the exact same vignettes, making it difficult to benchmark performance accurately.
5.2. Digital Literacy and Health Equity Disparities
The equitable distribution and utilization of digital health tools, including self-triage platforms, face significant challenges related to digital literacy and existing health disparities:
User Demographics: Analysis of user demographics consistently reveals that individuals who utilize online symptom checkers are often younger, female, possess higher levels of formal education, and are more technologically literate. This demographic skew contributes directly to the digital divide, potentially exacerbating existing health inequities. Older patients or those with lower educational attainment, for instance, tend to rely more frequently on traditional telephone triage or direct in-person contact.
Access Barriers: Significant barriers to equitable access include limited broadband internet access, low levels of digital literacy, and cultural mismatches in technology design that fail to resonate with diverse populations. The presence of medical jargon within the tools themselves can also hinder comprehension and effective usage for individuals with lower health literacy.
Exacerbating Disparities: If these pervasive disparities are not proactively and intentionally addressed, the increasing reliance on digital health tools risks widening existing health gaps, creating a two-tiered healthcare system based on technological access.
Frameworks for Equity: Recognizing this challenge, initiatives such as the Digital Health Care Equity Framework (DHEF) emphasize addressing "digital determinants of health." This involves tackling fundamental infrastructure challenges like broadband access, promoting digital literacy programs, advocating for participatory design that includes diverse communities, and mandating alternative access methods (e.g., phone-based sign-ups alongside digital options) to ensure equitable access for all populations. The consistent finding that self-triage tool users are skewed towards more privileged demographics, coupled with the explicit recognition of "digital determinants of health," elevates digital access and literacy to the status of a critical social determinant of health. This implies that without intentional, equitable design and deployment strategies, digital health innovations, while beneficial for some, risk exacerbating existing health disparities.
5.3. Patient Acceptance and Compliance
While patient satisfaction with self-triage tools is generally high, nuances exist regarding actual compliance and underlying reservations:
General Satisfaction: Patients typically report high levels of satisfaction with symptom checkers, perceiving them as easy to use and useful. They often express a general willingness to use these tools on a recurring basis. For example, 80% of Symptomate users indicated a likelihood to use the tool again.
Compliance Limitations: Despite high reported satisfaction, evidence regarding actual patient compliance with digital triage advice is limited. While the
intention to comply is often high (e.g., 65% for the "Should I see a doctor?" app) , patients may be apprehensive to follow advice perceived as excessive, largely due to the risk-averse nature of most tools. However, some data suggests significant shifts in patient plans after using virtual triage, with 83.9% changing their initial care plans and 62.2% opting for less urgent care options.
Reservations: Underlying concerns about data privacy and trust continue to pose obstacles to full patient acceptance and widespread adoption.
Preference for Human Interaction: The speed and convenience offered by automated systems can sometimes come at the cost of the ability to clarify and interpret responses through direct interaction with a medical professional. Some users may prefer this human element. Additionally, certain patients may prefer traditional internet search engines or established telephone services over rigid algorithmic questionnaires, valuing perceived freedom in describing symptoms.
5.4. Inherent Limitations: Inability to Perform Physical Examination
A fundamental and irreducible limitation of self-triage tools is their inherent inability to incorporate physical examination findings. Crucial diagnostic information derived from visual assessment (e.g., skin color, swelling, rashes), palpation (e.g., tenderness, masses), and auscultation (e.g., heart, lung, or bowel sounds) simply cannot be captured through a digital questionnaire. Many diagnoses cannot be definitively made without a hands-on physical examination. This inherent limitation underscores that these tools are primarily designed as triage systems—guiding patients to the appropriate level of care—rather than comprehensive diagnostic instruments. Reputable symptom checkers explicitly state this disclaimer, emphasizing their role as a complement to, not a replacement for, professional medical assessment by a trained healthcare provider.
Table 3: Challenges and Limitations of Self-Triage Tools
6. Ethical, Legal, and Regulatory Landscape
The integration of AI-driven self-triage tools into healthcare systems introduces a complex array of ethical, legal, and regulatory considerations that must be meticulously addressed to ensure responsible and safe deployment.
6.1. Privacy and Data Security Considerations
A paramount concern in the deployment of AI-powered self-triage tools is the privacy and security of sensitive patient data. These AI systems require vast volumes of data, including comprehensive medical histories, diagnostic imaging, laboratory results, and personal details, for effective learning and operation. This data, often stored in Electronic Health Records (EHRs), must be rigorously protected. Compliance with stringent data protection regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. and the General Data Protection Regulation (GDPR) in Europe, is not merely advisable but legally mandatory. Any breach or misuse of this sensitive information can lead to severe legal repercussions, substantial financial penalties, and a profound erosion of public trust in digital health solutions.Healthcare organizations are therefore obligated to implement robust security measures, including advanced data encryption, strict access controls, secure data storage protocols, and regular, comprehensive staff training to prevent breaches. Furthermore, any cloud services utilized for AI operations must adhere to equally stringent security rules to safeguard against unauthorized access by malicious actors.
6.2. Addressing Algorithmic Bias and Ensuring Inclusivity
A significant ethical challenge lies in the potential for AI algorithms to inadvertently perpetuate or even amplify existing biases within healthcare. This can occur if the data used to train these AI models does not adequately represent diverse patient populations. Such biases can lead to unfair or less accurate assessments and treatment recommendations for specific demographic groups. For example, a dermatology application was reported to perform ineffectively on Black or Brown skin, illustrating how biased training data can reinforce existing disparities in medical representation. Developers and healthcare providers bear a critical responsibility to proactively identify, mitigate, and continuously monitor for such biases throughout the AI lifecycle. This ongoing vigilance is essential to ensure that the care provided is equitable and inclusive for all individuals, regardless of their background.
6.3. Liability and Transparency ("Black Box" Concerns)
A particularly challenging aspect of AI integration is the "black box" nature of some AI systems, where the internal decision-making process is opaque and difficult for human users to comprehend. This lack of explainability hinders effective auditing, undermines trust, and complicates accountability when errors occur. Clinicians and patients alike need to understand and trust the advice generated by AI. There are legitimate concerns among medical professionals regarding liability, especially if adverse outcomes arise when AI has assisted in clinical decisions, and the human clinician does not fully understand the AI's rationale or who bears ultimate responsibility for the outcome. The "black box" problem directly threatens the foundational trust between patients and clinicians. If the reasoning behind a triage recommendation is unclear, it becomes difficult to ensure adherence to core ethical principles such as beneficence (doing good) and non-maleficence (avoiding harm). This situation necessitates a proactive commitment to explainable AI (XAI) to foster transparency and accountability, moving beyond mere performance metrics to a deeper understanding of how decisions are reached. Some jurisdictions, such as the UK, have already begun establishing clear rules for AI transparency and responsibility within their health systems.
6.4. Evolving Regulatory Frameworks
While existing legal frameworks, like HIPAA, provide a foundation for patient privacy, specific regulatory frameworks tailored to AI in healthcare are still in active development and evolving rapidly. In the U.S., the Food and Drug Administration (FDA) is actively developing pathways for the approval of AI medical devices and software. However, these approval processes can be slow and complex, often struggling to keep pace with the rapid advancements in AI technology. The FDA's Digital Health Center of Excellence aims to foster responsible innovation and provide efficient oversight for digital health technologies, including Software as a Medical Device (SaMD) and AI/Machine Learning in SaMD. The FDA has issued guidance documents covering various aspects, such as cybersecurity, AI-enabled device software functions, and clinical decision support software. Concurrently, international bodies like the World Health Organization (WHO) are developing classification frameworks to promote a standardized language for digital health interventions, which aids in evidence synthesis and strategic planning across global health initiatives. The contrast between the rapid pace of AI development and the slower, more complex nature of regulatory approval creates a "regulatory lag." This lag can either impede innovation by creating uncertainty for developers or risk the deployment of insufficiently vetted tools. This highlights a critical need for regulatory bodies to adopt more agile, adaptive, and collaborative governance models, as suggested by the FDA's objectives, that can effectively keep pace with technological advancements while simultaneously ensuring patient safety and upholding ethical standards.
7. Real-World Applications and Case Studies
Self-triage tools have demonstrated considerable utility across a diverse range of healthcare settings, gaining particular prominence and proving their value during recent public health crises.
7.1. Deployment in Diverse Healthcare Settings
These tools are being integrated into various facets of healthcare delivery:
Primary Care: Digitally enabled "total triage" systems have seen widespread adoption in general practice, particularly during the COVID-19 pandemic. These systems remotely screen all patient requests before directing them to the most appropriate care pathway. These tools can effectively supplement or even replace traditional telephone triage lines, optimizing patient flow and reducing administrative burden.
Emergency Medicine: Self-triage tools play a crucial role in alleviating demand and congestion in emergency departments (EDs). They guide patients with non-emergent issues towards alternative, more appropriate care settings. Furthermore, they significantly improve the likelihood of patients making correct urgent care choices for serious symptoms, thereby enhancing patient safety.
Pandemic Response: The COVID-19 pandemic served as a major catalyst for the mass-scale deployment of patient-facing digital self-triage tools across numerous countries. For instance, in France, 13 million questionnaires were completed within the first eight months of the pandemic, and a tool developed in Korea was accessed over 100,000 times in a four-week period across 141 countries. These tools were instrumental in managing increased patient numbers and alleviating the strain on acute care services. The widespread and mass-scale deployment of self-triage tools during the COVID-19 pandemic served as an unplanned, large-scale stress test for these technologies. Their demonstrated ability to manage surges, reduce emergency room congestion, and provide guidance on a mass scale validated their critical role not only in routine care but also in public health crisis management, firmly establishing their position as an essential component of modern healthcare infrastructure.
Chronic Disease Management: Patient self-management tools are increasingly utilized to help individuals manage long-term health conditions outside traditional formal institutions. These encompass a range of solutions, including home monitoring and messaging systems for tracking vital signs (e.g., blood pressure, glucose, weight), decision support aids, online interventions for behavior change, and online support groups that provide continuous assistance and encouragement. The successful application of self-triage tools in chronic disease management, enabling home monitoring and continuous self-management, signifies a broader systemic shift in healthcare. This moves healthcare beyond a purely reactive, acute care model to one that is increasingly proactive, preventative, and continuously engaged with patients in their daily lives, with profound implications for long-term health outcomes and the sustainability of healthcare systems.
Call Centers: Medical triage tools are effectively employed in dynamic call center environments to support agents. They significantly reduce the time required to find information and consequently cut down patient call wait times, leading to improved patient satisfaction.
7.2. Illustrative Case Studies
Several real-world implementations highlight the tangible impact of self-triage tools:
CARTI's Call Center Efficiency: By integrating decision tree software, CARTI achieved a remarkable reduction in call wait times, from highs of 20 minutes to an average of just two minutes. This demonstrates substantial gains in operational efficiency and improved patient access.
Infermedica's Virtual Triage Impact: Data from Infermedica's AI system revealed that 83.9% of patients altered their initial care plans after using virtual triage. Specifically, this led to a 35.7% decrease in patients intending to seek emergency care and a notable 56.5% increase in those choosing self-care options, effectively redirecting patients to more appropriate and less acute care settings.
"Should I See a Doctor?" App (Netherlands): A self-triage application developed in the Netherlands demonstrated high user satisfaction and a strong intention to comply with its recommendations. 65% of users intended to follow the app's advice, and in 81% of cases, the app's advice aligned with the outcome of a subsequent triage call, underscoring its practical utility and safety in real-world scenarios.
Australian Nurse Call Centers: The successful integration of virtual triage tools into nurse call centers in Australia resulted in a significant 50% reduction in emergency calls, showcasing the potential for substantial system-wide impact in managing demand and optimizing resource utilization.
Kaiser Foundation Hospitals: This prominent healthcare organization is actively developing a machine learning-based triage tool. The objective is to predict the severity of patient illnesses, illustrating the ongoing commitment to innovation and leveraging advanced analytics to improve care delivery and resource efficiency.
8. The Future of Self-Triage: AI, Personalization, and Predictive Analytics
The trajectory of self-triage tools is deeply intertwined with the ongoing advancements in Artificial Intelligence, promising a future characterized by increasingly personalized and proactive healthcare delivery.
8.1. Advancements in AI and Machine Learning for Improved Accuracy and Personalized Guidance
Artificial Intelligence and machine learning are poised to continuously enhance the accuracy and personalization capabilities of self-triage tools. As AI systems mature, their ability to interpret complex patient-reported symptoms and accurately predict health issues will improve significantly, leading to better patient outcomes. The adaptation of generalist AI models, such as Large Language Models (LLMs), for specialized medical applications through targeted training and sophisticated prompt optimization, holds immense promise for refining diagnostic accuracy and ensuring patient safety.The future will focus on developing AI frameworks that are not only highly effective but also trusted, explainable, and interoperable. This will support seamless integration across diverse clinical, operational, and research settings globally, fostering a more cohesive digital health ecosystem.
8.2. Integration with Predictive Analytics for Proactive Care
The integration of AI with predictive analytics represents a fundamental shift in healthcare, moving beyond reactive care models. These advanced models will enable healthcare systems to proactively estimate the probable course of an illness and its potential impact, identify and prioritize patients at risk of readmission, and develop highly individualized treatment strategies. This proactive approach allows for the creation of care plans and the strategic allocation of resources in advance, ensuring that patient-specific care is initiated before a potential deterioration of their condition occurs.Investments in AI-driven predictive modeling have already demonstrated tangible economic benefits, with hospitals reporting reductions in readmission rates by 15-20% and trimming operational costs by approximately 25%. The shift from current self-triage tools, which primarily react to symptoms to guide immediate care, towards future models integrating AI and predictive analytics, represents a fundamental paradigm shift. This evolution moves beyond mere symptom assessment to proactive health management, where AI anticipates illness progression, identifies at-risk groups, and enables individualized, preventative interventions. This transforms the role of these tools from simple "checkers" to sophisticated "forecasters" of health needs. As AI's role expands into predictive analytics and personalized medicine, the ethical considerations of bias, transparency, and accountability become even more critical. If AI is proactively recommending treatment strategies or predicting illness courses, any inherent biases or lack of explainability could have amplified negative consequences on patient equity and trust. This emphasizes that ethical design and robust regulatory oversight are not merely compliance issues but foundational requirements for the responsible and successful realization of AI's future potential in self-triage.
8.3. Potential for Enhanced Interoperability and Seamless Patient Journeys
The successful future of these technologies is contingent upon robust teamwork and close collaboration among administrators, IT staff, clinicians, and technology providers. Enhanced interoperability with existing Electronic Health Records (EHRs), patient portals, and scheduling programs will create smoother workflows, significantly reduce errors, and ensure a seamless patient journey from the initial triage assessment to definitive care delivery. The overarching objective of these advancements is to leverage AI to not only improve patient outcomes but also to manage healthcare costs more effectively, thereby contributing to a more sustainable and accessible healthcare system.
9. Recommendations for Stakeholders
To fully realize the transformative potential of patient empowerment through self-triage tools, a multi-faceted and collaborative approach involving all key stakeholders is essential.
9.1. Strategies for Effective and Ethical Implementation
Healthcare organizations must adopt a strategic framework that prioritizes both technological integration and ethical responsibility:
Prioritize Ethical Guidelines and Patient Privacy: Organizations must rigorously select and implement AI tools that adhere to stringent privacy regulations such as HIPAA and GDPR. This includes establishing clear security protocols, conducting regular data audits, and implementing robust data protection measures to safeguard sensitive patient information.
Address Bias and Ensure Inclusivity: It is imperative to proactively identify and mitigate algorithmic bias by ensuring that AI training data is diverse and truly representative of all patient groups. Continuous monitoring for unfair outcomes is crucial, requiring close collaboration with vendors who provide transparent explanations of their AI's functionality and data sources.
Plan for Seamless Integration: New AI tools must be designed for smooth and efficient integration with existing Electronic Health Records (EHRs) and other IT systems. This foresight prevents workflow interruptions, significantly reduces manual data entry, and improves the overall patient flow within the healthcare system.
Educate Staff and Clinicians: Comprehensive training programs are vital to equip healthcare staff and clinicians with a thorough understanding of AI tools' strengths, limitations, and appropriate use. Involving medical professionals early in the adoption process fosters their support and ensures effective human-AI collaboration, which is critical for successful implementation.
Adopt a Patient-Centered Approach: Tools should be designed with customizable input options to facilitate accurate symptom description and must provide clear, unambiguous language with comprehensive explanations of recommendations. This enhances the user experience and builds patient trust.
Ensure Continuous Monitoring and Review: Establishing robust mechanisms for ongoing monitoring and review of AI tool performance in real-world patient care settings is crucial. This includes processes to quickly address any identified issues, inaccuracies, or unintended consequences. The repeated emphasis on teamwork between administrators, IT staff, clinicians, and technology providers is not merely a best practice but a foundational requirement for successful digital health integration. The complexity of AI-driven self-triage transcends traditional departmental silos, demanding a shared understanding, coordinated effort, and continuous dialogue across these diverse domains to ensure that technological solutions are clinically sound, ethically robust, and operationally feasible.
9.2. Suggestions for Policy and Regulatory Development
Policymakers and regulatory bodies play a pivotal role in shaping the environment for responsible innovation:
Develop Adaptive Regulatory Frameworks: Regulatory bodies, such as the FDA, must create agile and responsive frameworks that can keep pace with rapid technological advancements in AI while consistently ensuring patient safety and efficacy.
Establish Standardized Datasets and Evaluation: Encouraging the development and use of standardized, diverse datasets for training and validating AI models is essential. Furthermore, promoting standardized methodologies for evaluating the accuracy and safety of self-triage tools will enhance comparability and reliability across different solutions.
Mandate Transparency and Responsibility: Clear regulations are needed to mandate AI transparency, often referred to as "explainability," ensuring that the decision-making processes of AI systems are comprehensible. Furthermore, clear lines of liability for clinical decisions made with AI assistance must be delineated.
Bridge the Digital Divide: Policies and allocated resources are necessary to address infrastructure challenges, such as limited broadband access, and to promote digital literacy programs. Mandating alternative access methods alongside digital tools will ensure equitable access for all populations, preventing the exacerbation of existing health disparities.
9.3. Guidance for Fostering Patient Trust and Engagement
Building and maintaining patient trust is paramount for the successful adoption and long-term impact of self-triage tools:
Communicate Role and Limitations Clearly: Healthcare providers and tool developers must be transparent with patients about the precise purpose of self-triage tools. It should be explicitly communicated that these tools are for guidance and triage, not definitive diagnosis, and that they do not replace professional medical assessment by a human clinician.
Involve Patients in Design: Implementing participatory design processes, where diverse patient communities are actively involved in the development and refinement of self-triage tools, is crucial. This ensures that the tools are culturally relevant, user-friendly, and genuinely address real-world patient needs.
Provide Comprehensive Explanations: Tools should be designed to offer clear, understandable explanations for their recommendations, allowing patients insight into the decision-making process. This transparency fosters greater confidence and trust in the tool's guidance.
Promote as Complementary Tools: Self-triage tools should be consistently positioned as valuable complements to traditional care, enhancing patient engagement and access, rather than as replacements for human clinicians.
Proactive and adaptive regulatory frameworks that effectively balance innovation with safety, coupled with transparent and ethical AI development practices, can create a virtuous cycle. By reducing uncertainty for developers and providers, these measures encourage responsible investment and deployment, which, in turn, builds greater public trust and patient acceptance. This increased trust then fuels broader adoption, providing more data for AI refinement and further driving innovation, ultimately leading to more effective and equitable self-triage solutions.
Case Studies: Successes and Lessons Learned
Several healthcare organizations have implemented patient self-triage tools with valuable outcomes and insights. Kaiser Permanente's implementation of an integrated self-triage platform represents one of the most comprehensive and successful case studies. After identifying increasing emergency department utilization for non-urgent conditions as a strategic challenge, Kaiser deployed a custom-developed triage tool accessible through their patient portal and mobile application. The system was carefully integrated with their appointment scheduling and telehealth platforms, creating seamless pathways between assessment and care. Within 18 months of full implementation, they documented a 27% reduction in emergency department visits for low-acuity conditions, 18% increase in virtual care utilization, and 92% patient satisfaction rates. Key success factors included extensive clinical validation before deployment, careful integration with existing digital ecosystem, and comprehensive staff education to ensure appropriate support for patients questioning algorithmic recommendations. The organization emphasized the importance of their phased implementation approach, beginning with lower-risk conditions before expanding to more complex presentations.
Intermountain Healthcare took a different approach, partnering with a commercial vendor to implement a white-labeled triage solution. Their experience highlighted important considerations around customization and local adaptation. After initial deployment showed lower-than-expected utilization and some clinical pathway misalignments, they conducted extensive revisions to adapt the tool to their specific patient population needs and available services. The revised implementation achieved much stronger results, with particular success in rural communities where patients reported that the tool helped them make more informed decisions about when lengthy travel to care facilities was warranted. Their experience underscores the importance of localizing algorithms to reflect specific organizational context rather than relying entirely on vendor defaults. The Cleveland Clinic's implementation offers insights into demographic adoption challenges, as their initial deployment showed strong uptake among younger patients but limited utilization among older adults who often have greater healthcare needs. Their subsequent targeted outreach and education campaign, including in-person demonstrations at senior centers and simplified interface options, significantly improved adoption among older patients. These diverse experiences illustrate both the potential benefits of self-triage implementation and the importance of thoughtful adaptation to specific organizational needs and patient populations.
Ethical and Health Equity Considerations
Patient self-triage tools raise important ethical and health equity considerations that healthcare organizations and developers must thoughtfully address. Potential exacerbation of existing healthcare disparities represents one of the most significant concerns, as research indicates uneven adoption and effectiveness across demographic groups. Lower utilization rates are consistently documented among elderly populations, those with limited digital literacy, individuals with lower socioeconomic status, and communities with limited broadband access. When self-triage tools become significant access points for care navigation, these adoption disparities risk creating additional barriers for already underserved populations. Performance disparities across demographic groups present another challenge, with some tools showing differential accuracy based on factors like primary language, cultural expression of symptoms, gender, and age. These variations risk perpetuating or even amplifying biases present in the healthcare system if not specifically addressed through inclusive design, diverse development teams, and rigorous testing across population groups.
Ethical implementation requires healthcare organizations to consider these tools within a broader context of comprehensive access strategies rather than as replacements for traditional entry points. Organizations leading in this space emphasize the importance of maintaining multiple access pathways including phone-based triage, in-person options, and special accommodations for vulnerable populations. Privacy and data governance considerations loom large as well, particularly as tools collect increasingly sensitive health information. Questions around appropriate secondary uses of self-reported symptom data, consent models for algorithm improvement, and potential commercialization of insights gained from these platforms require careful ethical frameworks and transparent communication with users. Healthcare organizations should establish clear data governance policies that prioritize patient privacy and autonomy while enabling appropriate quality improvement activities. Responsible implementation also includes monitoring for unintended consequences, such as potential delays in care for serious conditions that present atypically or are not well-captured by algorithmic assessment. These ethical considerations should not discourage innovation but rather guide the development of more inclusive, equitable self-triage ecosystems that enhance rather than restrict access to appropriate care.
Future Directions and Innovations
The landscape of patient self-triage tools continues to evolve rapidly, with several emerging technologies and approaches promising to address current limitations and expand capabilities. Multimodal assessment represents one of the most promising frontiers, moving beyond text-based symptom reporting to incorporate additional data inputs. Advanced platforms are beginning to integrate imaging capabilities that allow patients to photograph visible symptoms such as rashes or injuries, with computer vision algorithms assisting in analysis. Voice analysis technologies show potential for detecting subtle vocal biomarkers associated with conditions ranging from respiratory infections to neurological disorders. Some cutting-edge systems are developing integration capabilities with consumer health devices and wearables, incorporating objective measurements like heart rate, blood oxygen levels, and activity patterns alongside subjective symptom reports to enhance assessment accuracy. These multimodal approaches hold particular promise for improving assessment of conditions that benefit from visual or physiological data points beyond verbal symptom description.
Integration with longitudinal health records represents another significant development direction, with self-triage tools evolving from isolated assessment moments to components of continuous health monitoring and management. Emerging platforms incorporate historical patient data from electronic health records to create more personalized baselines and detect meaningful changes from individual norms rather than population averages. Advanced systems are beginning to implement sophisticated risk stratification models that consider not just current symptoms but comprehensive health profiles including chronic conditions, medications, social determinants, and past utilization patterns. The convergence of self-triage with remote patient monitoring creates opportunities for more proactive intervention, potentially flagging concerning trends before patients would traditionally seek care. As natural language processing capabilities continue to advance, next-generation tools will likely offer increasingly conversational interfaces that adapt to individual communication styles and health literacy levels, potentially reducing current disparities in tool effectiveness across demographic groups. These technological advances, coupled with growing implementation experience and outcomes research, suggest that patient self-triage will play an increasingly central role in healthcare navigation and delivery models over the coming decade.
Conclusion
Patient empowerment through self-triage tools represents a significant advancement in healthcare, fundamentally reshaping how individuals interact with and manage their health. These digital innovations, ranging from sophisticated AI-driven virtual triage systems to comprehensive symptom checkers, have demonstrated a remarkable capacity to enhance patient autonomy, improve health literacy, and facilitate more meaningful shared decision-making with clinicians. The benefits extend across the entire healthcare ecosystem, yielding enhanced convenience and appropriate care guidance for patients, streamlined workflows and reduced administrative burdens for providers, and substantial cost savings and optimized resource allocation for healthcare systems. The rapid, mass-scale deployment during the COVID-19 pandemic underscored their critical role in managing demand and highlighted their potential for transforming healthcare delivery from a reactive to a more proactive and preventative model.
However, the journey towards widespread and optimal integration of self-triage tools is not without its complexities. Persistent challenges related to diagnostic and triage accuracy, particularly the tendency towards overtriage and the inherent limitations in performing physical examinations, necessitate ongoing refinement and validation. Furthermore, the pervasive digital divide, characterized by disparities in digital literacy and access, poses a significant threat to health equity, demanding intentional strategies to ensure inclusivity. Concerns regarding patient acceptance, particularly around data privacy and the "black box" nature of some AI algorithms, underscore the critical importance of transparency and trust.
The future of self-triage is inextricably linked to the continuous evolution of Artificial Intelligence and its integration with predictive analytics. This promises a future of increasingly personalized guidance and proactive health management, where AI anticipates health needs and optimizes care pathways. Realizing this transformative potential hinges on a concerted, collaborative effort from all stakeholders. This includes healthcare organizations prioritizing ethical AI implementation, addressing algorithmic biases, and ensuring seamless integration with existing systems. Policymakers must develop adaptive regulatory frameworks that balance innovation with rigorous safety standards and actively work to bridge the digital divide. Most importantly, fostering patient trust and engagement requires clear communication about the tools' capabilities and limitations, active patient involvement in design, and positioning these technologies as valuable complements to, rather than replacements for, human clinical care. By embracing these recommendations, the healthcare sector can confidently navigate the complexities of digital transformation, truly empowering patients and revolutionizing access to high-quality, equitable care for all.
FAQ Section
Here are answers to frequently asked questions about patient self-triage tools:
What are patient self-triage tools? Patient self-triage tools are digital platforms that help individuals assess their symptoms, determine appropriate levels of care, and navigate healthcare systems. These range from simple symptom checkers to sophisticated AI-powered applications that analyze complex symptom patterns and provide personalized care recommendations based on clinical algorithms.
How accurate are patient self-triage tools? Current self-triage tools demonstrate variable accuracy levels, typically ranging from 65-85% when compared to clinical assessment. Leading platforms show higher accuracy for common conditions (75-85%) but significantly lower performance for rare diseases and complex presentations (40-60%). Most tools prioritize sensitivity over specificity, tending to recommend higher levels of care when uncertain.
What are the main benefits of patient self-triage tools? The main benefits include 24/7 immediate access to health guidance, reduced anxiety through clear information, education about symptoms and appropriate responses, reduced unnecessary emergency visits (15-30% reduction in studies), more efficient healthcare resource utilization, and particular value during infectious disease outbreaks for managing surge capacity.
What are the primary limitations and risks of self-triage tools? Primary limitations include inability to perform physical examinations, variable accuracy across different conditions, potential undertriage of serious conditions with subtle presentations, demographic performance disparities, accessibility barriers for elderly and low digital literacy populations, and privacy/security concerns regarding sensitive health information.
How do self-triage tools impact emergency department utilization? Studies show that effective self-triage implementation reduces non-urgent ED visits by 15-30% and redirects patients to appropriate settings like primary care, urgent care, or virtual visits. However, some tools may increase ED utilization through overtriage, especially for certain symptoms. The net impact depends on tool quality, implementation approach, and integration with care navigation systems.
What demographic groups benefit most from self-triage tools? Young adults (18-34) show highest adoption rates (60-75%) and satisfaction scores (4.5+/5). Patients with chronic conditions benefit from condition-specific tools that help distinguish routine symptoms from complications. Working parents value the convenience for initial assessment of children's symptoms. Rural populations with limited healthcare access gain particular value from remote assessment capabilities.
What implementation considerations are most important for healthcare organizations? Critical implementation factors include establishing clear clinical governance structures, customizing algorithms to reflect local clinical pathways, integrating with existing digital ecosystems (scheduling, patient portals, EHRs), comprehensive clinical validation, staff education, liability/legal review, and ongoing safety monitoring with defined incident response protocols.
How can healthcare organizations measure the success of self-triage implementations? Key performance indicators include clinical accuracy rates (compared to professional assessment), appropriate utilization impacts (ED/urgent care visits for non-emergent conditions), patient satisfaction and trust metrics, adoption rates across demographic groups, completion rates for self-assessment flows, follow-through rates on recommendations, and return on investment calculations including resource optimization.
What features make self-triage tools more effective? The most effective tools feature conversational interfaces using plain language, personalization capabilities that adapt to user demographics and history, clear explanations of reasoning behind recommendations, multiple language support, accessibility design for users with disabilities, seamless integration with appointment scheduling and telehealth options, and transparent communication about tool limitations.
How is AI transforming patient self-triage capabilities? Advanced AI is enabling more sophisticated symptom analysis through natural language processing that understands conversational descriptions, personalized risk assessment incorporating demographic factors and medical history, continuous learning from outcomes to improve recommendations, multimodal interactions including voice and image analysis, and integration with remote monitoring data for more comprehensive assessment.
Additional Resources
For readers interested in exploring patient self-triage tools further, the following resources provide valuable insights:
"Digital Front Doors: Patient Self-Triage and Navigation in the Age of Consumer Healthcare" by the NEJM Catalyst (2023) – This comprehensive report examines the strategic implications of digital self-triage implementation within broader digital transformation initiatives, including case studies from leading healthcare organizations and practical governance frameworks.
Patient Self-Assessment Tools Implementation Guide by the American Telemedicine Association (2023) – This practical resource provides detailed guidance for healthcare organizations planning self-triage implementations, including technical requirements, clinical validation approaches, and change management strategies.
"Symptom Checkers: A Critical Appraisal of Their Benefits and Limitations for Clinical Practice" in JAMA Internal Medicine (2024) – This peer-reviewed analysis provides a balanced examination of the current evidence base supporting self-triage tools, highlighting both proven benefits and areas requiring further research and development.
The Digital Health Consumer Adoption Report by Rock Health (2023) – This annual research report tracks consumer adoption trends for various digital health tools, with detailed sections on symptom checkers and triage platforms across demographic segments and condition categories.
"Health Equity in Digital Navigation: Best Practices for Inclusive Self-Triage Implementation" by the National Health IT Collaborative for the Underserved (2023) – This essential resource focuses specifically on strategies to ensure self-triage tools enhance rather than exacerbate healthcare access disparities, with particular emphasis on design principles and implementation approaches for vulnerable populations.
