Ethical Decision-Making and Resource Allocation in Military Triage
The practice of military triage operates within a profound ethical chasm defined by the tension between individual medical necessity and collective mission utility. This conflict necessitates that the military physician adopts a position of "mixed agency" , obligated simultaneously by the traditional Hippocratic Oath.


The practice of military triage operates within a profound ethical chasm defined by the tension between individual medical necessity and collective mission utility. This conflict necessitates that the military physician adopts a position of "mixed agency" , obligated simultaneously by the traditional Hippocratic Oath (a deontological duty to the patient) and the strategic needs of the combat mission (a utilitarian mandate to the nation).
This report examines how this duality shapes triage protocols and resource allocation decisions. The analysis reveals a persistent incompatibility between the International Humanitarian Law (IHL) mandate, which demands care based solely on medical grounds without discrimination , and historical military doctrines that prioritize care based on status or return-to-combat potential. This tension places the medical professional in a position of enduring moral distress. Furthermore, the analysis of macro-level resource rationing, exemplified by the controversial allocation of penicillin during World War II, demonstrates that strategic utility often overrides individual clinical need when a resource becomes a critical military asset. Modern military medical policies must therefore seek a mixed ethical framework that legally preserves the non-discriminatory requirements of IHL while functionally addressing the logistical realities of wartime scarcity.
Defining the Battlefield Ethics Landscape
The ethical environment of military medicine is fundamentally shaped by the inherent paradox faced by the medical professional: the dual commitment to preserving life without distinction and ensuring the operational success of the fighting force. This duality is the principal source of ethical distress and is captured by the concept of "mixed agency".
The Functional Role of Triage as Logistics Optimization
Triage, in the military context, is not simply a clinical assessment but a highly structured resource allocation mechanism required by acute scarcity. Critical limitations exist not only in surgical capacity and personnel but also in specialized assets such as blood products and timely evacuation platforms. The calculus shifts dramatically from prioritizing "what is possible" in an ideal setting to prioritizing "what must be done to optimize collective survival and mission tempo."
The operational structure of casualty management formalizes this utilitarian efficiency. Roles such as the Medical Supervisor, who oversees coordination and patient resource allocation, and the Triage Officer, who coordinates patient flow to transport based on designated clinical condition, illustrate a system designed to manage logistical throughput. In this framework, the clinical condition of the patient—their objective medical need—serves primarily as an input variable for a larger logistical decision aimed at optimizing resource use and transportation flow. This structural design ensures that the military medical goal is systematically redefined, shifting from minimizing mortality generally to maximizing the fighting strength and capacity of the combat force.
The systematic requirement for medical professionals to operate under a standard that elevates mission success or military status over pure clinical urgency, as historical military thinking suggests , ensures that the potential for moral injury is embedded directly within the required doctrine. The professional is compelled to make trade-offs that violate the purely patient-centered focus of traditional medical ethics.
Theoretical Foundations of Military Medical Ethics
The profound dilemmas of military triage are rooted in the conflict between two fundamental moral philosophies: deontology and utilitarianism. Understanding this philosophical friction is essential to grasping the ethical demands placed on the military physician.
The Conflict of Moral Philosophies in Crisis
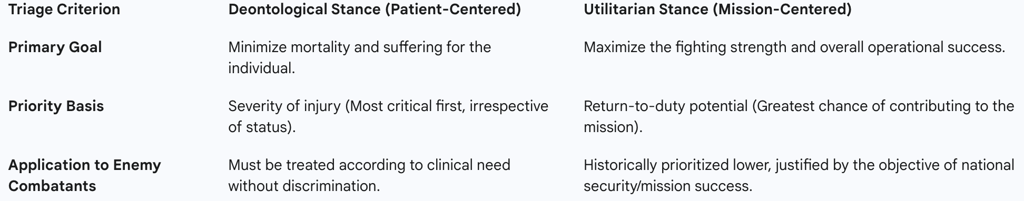
Deontological imperatives, which are patient-centered, dictate that morality rests on the nature of the action and adherence to duty, such as the Hippocratic Oath. Under this framework, the patient must be treated as an end in themselves, requiring care to be provided to the most seriously injured first, irrespective of their military status or their potential future utility.
Conversely, utilitarian mandates are mission-centered, judging the morality of an action by its consequences, specifically the maximization of the greatest happiness or welfare for the largest number of people, which, in the military, translates to the collective force. This consequentialist view justifies prioritizing patients based on the probability of a quick return-to-duty, as this action demonstrably serves the overarching goal of mission success and force preservation. The existence of competing ethical frameworks, even in civilian medical ethics debates during crises , suggests that current medical practices, particularly in mass casualty or pandemic scenarios, show an observed trend away from pure deontological adherence toward a utilitarian approach, which consistently creates professional frustration and discontentment.
The Concept of "Mixed Agency" and Dual Loyalty
The military doctor’s role is defined by their need to bridge the chasm between their commitment to providing unbiased medical care and their allegiance to national security. This "mixed agency" generates acute dual loyalty conflicts.
The most prevalent dilemma arises in priority of care. While International Humanitarian Law (IHL) explicitly requires care to be dispensed solely on medical grounds , traditional military thinking has often directed combat casualty care priority based on status: own troops first, allies second, civilians third, and the enemy fourth. Prioritizing based on nationality, political standing, or operational status directly contradicts the medical ethical principle that the most seriously injured casualty should be attended to first regardless of who they are.
The dual loyalty crisis is further compounded when medical skills are utilized for nonmedical ends. These situations include complicity in the abuse of medicine, using medical presence to achieve nonmedical aims like gaining intelligence, or leveraging medical aid for "winning hearts and minds" campaigns. Such instrumentalization compromises the fundamental neutrality required of medical personnel and undermines the trust essential to the profession.
The profound conflict between these philosophies is summarized in the following table, illustrating how the military context forces a consequential trade-off between the individual patient’s well-being and the collective force’s operational needs.
Table 1: Ethical Frameworks Applied to Combat Triage
Military Triage Doctrine and Its Ethical Consequences
The operational manifestation of the ethical conflict is visible in established military doctrine, where protocols aim to maximize survival and operational readiness under duress.
Current Triage Methodology and TCCC
Tactical Combat Casualty Care (TCCC) protocols embody a structured, utilitarian approach designed to provide immediate, high-yield interventions that address the fastest causes of preventable death, such as massive hemorrhage control and airway management, thereby optimizing survival rates with minimal resource expenditure in far-forward environments.
Standard military triage generally sorts casualties into three broad categories based on prognosis relative to available resources : 1) those who will survive without immediate extensive care; 2) those who will die if they do not receive immediate care; and 3) those who are unlikely to survive regardless of the medical resources expended
The Prioritization Dilemma: Utility as the Decisive Factor
In severely resource-constrained settings, the prioritization dilemma often sees operational utility outweighing clinical severity. For instance, personnel categorized as "Minimal" (Green tag) may receive prioritized treatment or rapid evacuation over more severely injured but stable casualties ("Delayed" or Yellow tag) if they can be quickly stabilized and returned to combat duty. This is a deliberate tactical choice focused on optimizing the overall operational outcome by maximizing the effective fighting force.
The ethically most challenging decision is the assignment to the "Expectant" category (Black tag). This designation is reserved for patients suffering from catastrophic injuries where survival is unlikely, irrespective of exhaustive medical intervention. This judgment is the purest application of utilitarian ethics in medicine: it requires the purposeful redirection of scarce, finite resources—surgical time, specialized medical personnel, blood products, and ventilators—to those patients who possess a higher probability of survival, thereby maximizing the number of saved lives collectively.
When military doctrine historically directed medical personnel to prioritize one’s own troops over an enemy combatant based purely on military status , the Triage Officer was placed in a legally precarious situation, as this directly conflicts with IHL’s demand for care based solely on medical need. Consequently, modern military casualty systems have undergone essential legal adaptations, moving away from explicit status-based prioritization to clinical-need-based protocols. However, the operational pressure in true crisis standards of care may still force a reversion to a status-based priority (treating a less-injured comrade over a more severely injured enemy) in a bid to satisfy line command and operational requirements, thereby creating an intense ethical and potentially legal violation of IHL.
Furthermore, the explicit "Expectant" category is sometimes minimized or omitted in public-facing policy documents. This indicates an institutional understanding that while withholding care in these crisis circumstances may be medically and strategically rational under crisis standards, the decision is fundamentally difficult to defend from a purely deontological standpoint, necessitating efforts to mitigate the moral burden on the practitioners.
Legal and Regulatory Constraints: International Humanitarian Law (IHL)
International Humanitarian Law, codified primarily in the Geneva Conventions, provides the essential deontological framework that legally constrains the application of operational utility in military medicine.
The Geneva Conventions and Non-Discrimination
The Geneva Conventions establish minimum protections and fundamental guarantees of respect for all individuals affected by armed conflict. Convention I, applicable to the wounded and sick in the field, and Common Article 3, applicable to non-international conflicts, mandate humane treatment and medical care without any adverse distinction.
The fundamental principle is that medical aid must be dispensed solely on medical grounds. This prohibition against adverse distinction specifically bars prioritization based on "sex, race, nationality, religion, political opinions, or any other similar criteria". This non-discrimination clause applies broadly, covering soldiers not actively participating in hostility, shipwrecked sailors (Convention II), and civilians (Convention IV). Therefore, IHL explicitly forbids prioritizing a soldier over a civilian, or a friendly combatant over an enemy combatant, based on their strategic utility to the mission. Priority must be determined by the urgency of the clinical condition.
Protections and Responsibilities of Medical Personnel
To protect this humanitarian standard, IHL grants special status to medical personnel. Medical personnel exclusively assigned to medical duties must be respected and protected in all circumstances. This requires that they "must not knowingly be attacked, fired upon, or unnecessarily prevented from discharging their proper functions".
Crucially, IHL also prohibits punishing medical personnel for providing medical assistance. This requirement acts as the primary legal defense of deontological principles in wartime. It furnishes military medical personnel with the necessary legal leverage to resist operational orders that would mandate violating core ethical tenets, such as participating in torture, or engaging in status-based triage. This protection is maintained unless the medical personnel commit acts harmful to the enemy outside of their humanitarian function.
The fundamental IHL requirement that care be based solely on clinical urgency renders any military triage protocol that explicitly uses "Return-to-Duty Potential" as the decisive sorting variable legally vulnerable. This necessitates a critical distinction: while operational utility can legitimately influence logistical and evacuation priority (i.e., who gets moved where next), it legally cannot override the determination of clinical priority or treatment order at the point of care.
Macro-Level Resource Allocation: The Historical Precedent of WWII Penicillin
The ethical dilemmas of resource allocation extend far beyond the battlefield triage decision to encompass strategic, macro-level rationing policies, as demonstrated by the controversial allocation of penicillin during World War II.
Penicillin as a Strategic Military Asset
The Allies immediately recognized penicillin's prodigious clinical effectiveness against bacterial infections, deeming it a drug of immense strategic military value. Mass production efforts were therefore centered on meeting the needs of the armed forces first and foremost.
Medical leaders publicly defended this operational priority. Sir Howard Florey, a key figure in penicillin research, publicly stated that it was "very right and proper" that the drug be reserved for the armed forces, citing its critical value in treating war wounds. This policy served the strategic goal of force preservation and provided assurance to the families of service members that life-threatening battle injuries could be countered.
The Military vs. Civilian Allocation Policies
The implementation of this strategic utility framework varied geographically. The British policy maintained strict utilitarian priorities, striving to ensure all military needs were met, effectively rendering penicillin unavailable to the civilian population for the duration of the conflict. The low rate of British production further reinforced the severity of the scarcity argument.
In contrast, the United States recognized the need to provide a limited buffer for civilian needs. The US system allocated a proportion of the drug for civilian patients suffering from intractable infections, managed under strict guidelines established by Chester S. Keefer. This micro-allocation system, although intended to address the gap, became the center of public controversy.
The Ethical Outcry and the "King Solomon Dilemma"
The knowledge that a "miraculous new drug" existed but was out of reach generated intense public frustration and despair among civilian sufferers, particularly those with infections resistant to existing treatments. Sections of the press magnified instances of human tragedy resulting from the rationing, notably the denial of penicillin to a desperately sick child who subsequently died.
Keefer’s role as the civilian resource allocator in the US came under intense scrutiny, resulting in press headlines concerning the "Heartbreaking King Solomon Dilemmas". This coverage framed the ethical dilemma for the public: choosing which civilian—soldier, sailor, child, or adult—must be allowed to face death so that others might live.
This historical episode crystallizes the conflict: the strategic utilitarian duty to win the war (force preservation) required the violation of the individual deontological duty (saving the desperately sick child). The controversy was fundamentally fueled by the juxtaposition of the drug’s publicized efficacy against the arbitrary denial created by centralized allocation. The prioritization of penicillin based on its instrumental value—its ability to return soldiers to the fight and maximize the military outcome—established a foundational precedent for resource allocation based on maximizing future societal or organizational contribution, a principle still seen today in modern crisis allocation models.
Policy Implications and Future Directions
The ethical lessons derived from military triage and historical rationing precedents hold significant relevance for contemporary medical policy, particularly under crisis standards of care.
Modern Resource Debates and Instrumental Prioritization
Modern medical crises, such as large-scale disease pandemics, necessitate rationing scarce critical resources, including ventilators, ICU capacity, and specialized blood products. These challenges resurrect the fundamental utilitarian arguments inherent in military triage.
The concept of maximizing instrumental or social value has re-emerged in civilian policies. For example, preferential allocation of critical care resources to health care workers is justified because maximizing their recovery maximizes the number of patients they can treat in the future. This rationale directly parallels the military objective of prioritizing return-to-duty potential to maximize the overall operational force.
In times when resources are critically low, and contingency or crisis standards of care are implemented, transparency becomes crucial. Clinicians are obligated to openly and clearly address conflicting interests with patients and surrogates, particularly concerning triage decisions that may lead to the deactivation of cardiac devices or the withdrawal of ventilators.
Ethical Policy Development and Training
To mitigate the acute strain of dual loyalty and prevent moral injury among military medical professionals, policy must focus on protecting them from the legal and moral consequences of operational pressure demanding utilitarian choices.
Comprehensive training is essential. This training must go beyond theoretical concepts and involve mandatory, scenario-based exercises that force reconciliation between the strict legal requirements of IHL (non-discrimination and the requirement to treat based solely on medical grounds ) and the reality of operational necessity. This approach ensures that medical personnel understand IHL as their primary legal defense against illegal orders, such as participating in status-based triage or nonmedical uses of medicine.
The Requirement for a Mixed Ethical Model
Moving forward requires the formal adoption of a "mixed ethical position" that acknowledges the limitations of adhering solely to utility or deontology in combat. The objective must be to achieve congruity between the collective mission and the rights of the individual patient.
This necessitates a crucial policy separation: Military triage protocols must formally delineate between the clinical severity assessment and the logistical evacuation priority. The clinical triage tag, which determines the urgency of immediate intervention, must be based solely on medical need to remain compliant with IHL. However, the logistical evacuation priority—the order in which casualties are moved from the point of injury to the next level of care—may incorporate mission-driven factors such as operational status, military rank, or return-to-duty potential. This dual approach respects the patient's humanitarian rights while satisfying the practical requirements of military strategy.
Balancing Duty, Humanity, and Strategy
The ethical environment of military triage is one of calculated compromise. The demands of warfare perpetually subject the sanctity of individual care to the strategic imperatives of the collective mission.
International Humanitarian Law serves as the indispensable legal barrier against the complete domination of utilitarian principles, providing an external, legally binding deontological floor that ensures human dignity and non-discriminatory treatment remain the baseline standard in conflict.
The enduring legacy of controversies such as the WWII penicillin allocation is a mandate for institutional transparency. Military medical authorities must continuously refine and publish ethically reasoned, legally defensible frameworks for resource rationing. These frameworks must honor the duty to the nation and the strategic necessity of the mission while firmly upholding the core duty to humanity, ensuring that the care provided is rooted in clinical urgency above all other criteria.
