AI Triage and Predictive Analytics for Optimized ED Flow
Discover how AI triage systems and predictive analytics are transforming emergency departments, reducing wait times by up to 30%, and improving patient outcomes through data-driven healthcare management.

Emergency Departments (EDs) worldwide operate as high-pressure, critical hubs within healthcare systems, frequently contending with persistent challenges such as overcrowding, extended wait times, and significant resource constraints. These systemic inefficiencies profoundly impact patient care quality, staff performance, and the financial viability of healthcare institutions. Artificial Intelligence (AI) and predictive analytics are rapidly emerging as transformative tools to address these issues, fundamentally reshaping patient flow and operational management within emergency care.
The integration of these advanced technologies offers substantial benefits. They significantly enhance patient prioritization, leading to notable reductions in wait times, and optimize resource allocation, encompassing crucial aspects like staffing and bed management. Furthermore, AI streamlines numerous administrative tasks, ultimately contributing to improved patient outcomes and heightened safety. Evidence suggests that AI-driven triage systems can reduce patient wait times by up to 30% , while the strategic application of predictive analytics has been shown to increase hospital income by 30% to 45% through optimized scheduling and reduced missed appointments.
Despite their immense promise, the widespread adoption of AI and predictive analytics in EDs faces several hurdles. These include the critical need to ensure high data quality and interoperability across disparate systems, effectively mitigating algorithmic bias, cultivating strong clinician trust, rigorously safeguarding patient data privacy, and managing the substantial upfront implementation costs.
Successful integration of these technologies necessitates a deliberate, phased approach, underpinned by robust data governance and comprehensive ethical frameworks. Continuous staff training and fostering interdisciplinary collaboration are also paramount to realizing the full potential of AI in emergency care. Looking ahead, AI is poised for deeper integration with innovations such as wearable health technology, digital twins for simulation, and the development of hyper-personalized care pathways. This trajectory promises to pave the way for a more agile, efficient, and patient-centric emergency medicine landscape.
Current Pressures and Inefficiencies in Emergency Departments
Emergency Departments globally are under considerable strain, often characterized by a confluence of persistent challenges that compromise their effectiveness. Overcrowding is a pervasive issue, leading to prolonged wait times and significant constraints on available resources. These operational bottlenecks are not merely inconveniences; they directly impede the quality of patient care, diminish staff performance, and can adversely affect a hospital's financial health.
Traditional triage methods, while foundational to emergency care, often rely heavily on the subjective clinical judgment of healthcare professionals. This reliance can introduce variability in decision-making, particularly under conditions of high workload pressure or during mass casualty events. Such inconsistencies in patient prioritization can lead to delayed treatment for critically ill individuals or the misallocation of scarce resources to less urgent cases. The inherent unpredictability and high-stakes nature of EDs amplify the negative impacts of these traditional inefficiencies. Any variability or delay, no matter how small, can cascade through the system, creating compounding delays and errors. For instance, inconsistent triage decisions, influenced by human variability, can result in patients receiving lower severity scores than appropriate, leading to delayed treatment and increased health risks. This dynamic can be understood as a "chaos multiplier," where existing operational instability is exacerbated by the very environment it seeks to manage.
The Strategic Role of AI and Predictive Analytics in Modernizing ED Operations
In response to these escalating challenges, Artificial Intelligence and predictive analytics are emerging as transformative approaches. These technologies offer a pathway to fundamentally address long-standing inefficiencies by enhancing the speed and accuracy of medical interventions. By leveraging vast datasets and advanced algorithms, AI enables data-driven decision-making, moving beyond the inherent limitations of subjective assessments to improve consistency and optimize resource allocation.
The strategic deployment of AI in emergency medicine is not intended to replace human experts but rather to augment their capabilities. AI-enabled medical technologies can execute certain tasks with greater consistency, speed, reliability, and reproducibility than human agents, thereby empowering clinicians with smarter tools for decision-making, reducing administrative burdens, and ultimately enhancing patient care. This capability to introduce consistency and data-driven predictability acts as a "chaos mitigator," directly addressing the core operational instability of EDs. By automating and standardizing processes, AI reduces the points of failure and variability that lead to systemic issues. The strategic role of AI is therefore not just optimization, but the establishment of fundamental operational resilience within the emergency care environment.
AI Triage and Predictive Analytics
AI- Triage
AI-driven triage represents a significant evolution in patient prioritization within the Emergency Department. It is defined as the process of assigning a degree of medical urgency to patients upon their arrival, utilizing real-time patient data—including vital signs, comprehensive medical history, and presenting symptoms—to automate and standardize the prioritization process. This approach moves beyond traditional triage methods, such as the Emergency Severity Index (ESI) or the Manchester Triage System (MTS), which primarily rely on clinical judgment and can be influenced by subjective factors, workload pressures, and variability among individual clinicians.
By rapidly analyzing multiple data points, AI-driven systems enhance consistency, optimize resource allocation, and are designed to reduce waiting times, particularly for critically ill patients, through precise risk stratification. An illustrative example is the Diagnostic AI System for Robot-Assisted ED Triage (DAISY) project, a collaborative effort between NHS England and the University of York. This system aims to automate elements of the ED triage process by collecting both subjective patient information and objective data via wirelessly connected medical devices (e.g., blood pressure, pulse rate, temperature, respiratory rate). DAISY then applies a complex, rule-based algorithm, "dAvInci," devised by medical experts, to link patient characteristics, demographics, and symptoms with objective vital signs. The system suggests possible early diagnoses, urgency levels, and further investigations for review, approval, amendment, or rejection by a medical practitioner, thereby streamlining the early stages of triage.
Predictive Analytics in Healthcare
Predictive analytics in healthcare involves the sophisticated application of machine learning models and statistical algorithms. These tools process vast amounts of real-time and historical patient data, such as electronic health records, vital signs, and laboratory results, to uncover intricate patterns and trends. The overarching objective of this process is to generate accurate predictions concerning individual health outcomes—including the probable course of a disease, potential adverse reactions to medications, or the risk of hospital readmission—as well as broader population-wide events, such as the anticipation of pandemics or surges in patient influx. This predictive capability empowers healthcare organizations to make highly informed, proactive decisions, enabling the personalization of care and the anticipation of health risks on a large scale.
Overview of Core Technologies and Algorithms
The efficacy of AI-driven triage and predictive analytics is rooted in several cutting-edge technologies and algorithms:
Machine Learning (ML): As the foundational technology, ML enables algorithms to learn from data and make predictions or decisions without explicit programming. In healthcare, ML is crucial for risk stratification, predicting disease severity, and identifying subtle clinical patterns that might be imperceptible through manual assessment.
Natural Language Processing (NLP): NLP empowers AI systems to comprehend, interpret, and generate human language. This is applied to patient narratives, chatbot interactions, digital intake forms, and clinical notes. NLP significantly facilitates automated documentation and the analysis of patient-reported symptoms.
Deep Learning: A specialized subset of ML, deep learning excels at analyzing complex, unstructured datasets, such as medical images (e.g., CT scans, X-rays) to detect subtle abnormalities, and for developing highly accurate forecasting models.
Specific ML Algorithms: Various algorithms are employed based on the specific predictive task:
Random Forest: Primarily used for classification and regression problems, this algorithm constructs an ensemble of decision trees by randomly sampling subsets of data. It is particularly well-suited for large datasets, allowing for parallel processing to save time.
Generalized Linear Model: An extension of the general linear model, it effectively analyzes the effects of multiple variables on continuous outcomes. It trains quickly and handles categorical predictors well, offering interpretability and resistance to overfitting, though it requires large datasets and can be susceptible to outliers.
Gradient Boosted Model: Similar to Random Forest, this model also uses an ensemble of decision trees but employs a "boosting" technique. It is highly valued for its accuracy and thorough data testing, consistently emerging as a top-performing algorithm in various healthcare predictive tasks, despite longer training times.
K-Means: A widely used clustering algorithm, K-Means groups unlabeled data points based on similarities. It is a high-speed algorithm beneficial for personalizing plans within large datasets.
Device Integration: The seamless incorporation of data from digital medical devices, wearable health technologies, and remote monitoring tools (e.g., smartwatches, portable ECG monitors, digital stethoscopes) provides AI systems with real-time objective data capture, crucial for dynamic patient assessment.
Machine Learning Operations (MLOps): This architectural framework is vital for facilitating continuous model updates, which significantly enhances forecast accuracy and ensures resilience against data drift—even in response to unforeseen events like pandemics or natural disasters. MLOps is essential for transitioning AI models from theoretical constructs to reliable and continuously performing tools in real-world clinical practice.
While AI is consistently positioned as a tool to support and augment human performance rather than replace human experts , a critical challenge arises from the nature of some advanced ML techniques, particularly deep learning. These models can often operate as "black boxes," where the internal logic for their predictions is not easily discernible. This opacity can create a significant barrier to adoption, directly impacting clinician trust and accountability. In regulated industries like healthcare, where decisions carry profound consequences, the inability to understand or justify an AI's output can lead to hesitation among medical professionals. For AI to truly augment and be widely adopted, healthcare organizations must strategically invest in or demand "explainable AI (XAI)" techniques. This ensures transparency, builds clinician confidence, and allows for informed human oversight, thereby aligning the technology with its intended role as a supportive tool rather than an unchallengeable oracle.
Optimizing ED Flow: Benefits and Impact
The strategic implementation of AI and predictive analytics in Emergency Departments yields a multifaceted array of benefits, profoundly impacting operational efficiency, patient care quality, and financial sustainability.
Reduced Wait Times and Enhanced Patient Throughput
One of the most immediate and impactful benefits of AI-driven triage systems is the significant reduction in patient wait times, particularly for critically ill individuals. By rapidly assessing and prioritizing patients based on urgency, AI streamlines the initial stages of emergency care. Studies indicate that AI-driven triage can reduce overall wait times by up to 30%. Other research has shown average wait time reductions of 18.7 minutes, and in some specific cases, a median waiting time for medical care was reduced from 1.97 hours to 0.38 hours with AI assistance. This streamlining of patient flow and expedited decision-making directly contributes to faster patient throughput within the ED.
Beyond initial triage, AI contributes to efficiency through virtual queuing and self-service technologies. Virtual lines and self-check-in kiosks reduce physical crowding in waiting rooms and accelerate the check-in process. For instance, Kaiser Permanente reported that approximately 75% of patients found kiosks faster than traditional clerks, with 90% able to check themselves in without assistance, thereby reducing front desk congestion. A notable case study from an unnamed medical center demonstrated the power of AI predictive tools and process changes, where the time for a patient to see a provider dropped dramatically from 59 minutes to 14 minutes, and the time to get a room decreased from 37 minutes to just 4 minutes.
Improved Patient Prioritization and Diagnostic Accuracy
AI systems excel at processing vast amounts of patient data in real-time, enabling more precise risk stratification. This capability allows for the early identification of patients at higher risk of deterioration, ensuring they receive timely and appropriate care. The ability of algorithms to detect early signs of time-sensitive conditions—such as strokes, sepsis, and cardiac events—is particularly beneficial, as early intervention in these cases significantly improves patient outcomes.
Furthermore, AI enhances diagnostic accuracy by analyzing extensive patient data and identifying subtle clinical patterns that might be overlooked during manual assessments. AI models have demonstrated superior diagnostic accuracy, with a pooled area under the receiver operating characteristic curve (AUC) of 0.88 in studies. AI-powered tools can also prioritize imaging data based on urgency, quickly flagging critical conditions like intracranial hemorrhage or pulmonary embolism, which accelerates the decision-making process for physicians. The ability of AI to rapidly identify high-risk patients and predict deterioration is not merely about speed; it fundamentally shifts the paradigm from reactive to proactive care. This early intervention, especially in time-sensitive conditions, creates a positive feedback loop: faster diagnosis leads to earlier treatment, which in turn leads to significantly improved patient outcomes and potentially reduced long-term care costs by preventing conditions from escalating.
Strategic Resource Allocation and Staffing Optimization
AI plays a pivotal role in optimizing resource allocation by dynamically adjusting patient prioritization based on real-time ED capacity and resource availability, thereby minimizing congestion and enhancing workflow efficiency. Predictive analytics is instrumental in forecasting patient demand, enabling hospitals to optimize staffing schedules, deploy additional staff during anticipated peak times, and proactively prepare resources to prevent overcrowding. For instance, the SO-SAFED system, an AI-driven forecasting and shift optimization tool, demonstrated its effectiveness by increasing physician allocation by up to 30.4% during peak hours and reducing the patient-to-physician ratio by an average of 4.32 to 4.40 patients per shift. AI also contributes to efficient bed management by predicting patient inflows and facilitating early discharge planning for stable patients, which can reduce extra hospital days by 15% to 30% and free up beds more quickly.
Streamlined Operations and Cost Efficiencies
The automation of routine administrative tasks by AI significantly streamlines operations and yields substantial cost efficiencies. These tasks include patient scheduling, staff scheduling, data entry, billing, and discharge planning, all of which free up clinicians' time for direct patient care. Automated scheduling tools have been particularly impactful, helping hospitals increase income by 30% to 45% by reducing missed appointments and expediting the filling of cancellations. AI-driven discharge planning, by estimating and planning early discharges, has been shown to reduce extra hospital days by 15% to 30%, which not only frees up beds but also accelerates patient movement through the system. By making patient stays shorter, speeding up admissions and discharges, and improving staff utilization, AI directly contributes to significant reductions in operational costs. Hospitals such as Boston Medical Center and HonorHealth have reported improved capacity management and reduced patient hospital time through the implementation of AI solutions.
Enhanced Patient Outcomes and Safety
The timely and efficient care facilitated by AI directly translates to better recovery rates and overall improved patient outcomes. Continuous monitoring through AI integrated with wearable health technology enables the early detection of deteriorating conditions and allows for proactive intervention, particularly in high-risk patients. AI-driven decision support systems provide physicians with actionable insights, assisting them in diagnosing and treating patients more efficiently. Furthermore, AI contributes to patient safety by reducing mis-triage rates (e.g., from 1.2% to 0.9%) and achieving high accuracy rates (AUROCs of 0.991) in patient assessment.
The benefits observed in ED operations are not isolated but are deeply interconnected. Operational improvements, such as faster patient throughput and automated administrative tasks, directly enable clinical benefits like better patient outcomes and reduced errors. For example, AI-driven scheduling and patient flow management lead to reduced wait times. These reduced wait times ensure that critical patients receive timely care, which in turn leads to better recovery rates. Similarly, the automation of administrative tasks reduces the manual workload for staff, freeing them to focus on direct patient care. This reduction in cognitive load can also lead to fewer errors. The optimization of bed occupancy ensures that beds are available for high-acuity cases, preventing resource misallocation. This synergistic relationship highlights that the true value of AI in EDs lies in its ability to create a more fluid and responsive system where operational efficiency directly underpins and enhances clinical quality and safety. This holistic improvement makes the investment in AI a strategic imperative for overall health system performance.
Navigating the Landscape: Challenges and Ethical Considerations
Despite the compelling benefits, the widespread implementation of AI in Emergency Departments is accompanied by significant challenges and ethical considerations that demand careful navigation.
Data Quality, Integration, and Interoperability
The effectiveness of AI models is profoundly dependent on the quality and quantity of data used for their training and decision-making processes. A primary hurdle is the pervasive issue of poor data quality, incompleteness, and fragmentation within healthcare systems. Patient data is often scattered across disparate sources such as Electronic Health Records (EHRs), laboratory systems, and insurance databases. Inconsistent formatting, varied coding practices, and incomplete records severely hinder the ability to extract reliable insights and can lead to inaccurate predictions from AI models. Moreover, integrating new AI solutions with existing, often outdated, hospital information systems (legacy systems) presents a substantial technical and organizational challenge, requiring significant investment and effort to ensure seamless data flow and avoid workflow disruptions.
Algorithmic Bias and Equity of Care
A critical ethical concern is the potential for AI models to inherit and perpetuate biases present in their training data. If the datasets reflect historical inequalities or prejudices, the AI can inadvertently lead to discriminatory outcomes or unfair treatment recommendations, particularly for marginalized populations. Research has demonstrated how human judgment biases, often linked to demographic factors such as sex, gender, age, and ethnicity, can influence traditional triage decisions. For example, studies have shown that female patients may be assigned lower severity ratings than male patients presenting with identical clinical conditions. AI models trained on such biased historical data are prone to reproducing these disparities. This bias can manifest as under-triage, where a patient receives a lower severity score than appropriate, leading to delayed care and increased health risks, or over-triage, which can strain hospital resources. The combination of AI's "black box" nature and the documented presence of algorithmic bias creates a significant "trust deficit" among clinicians and patients. This is not merely a technical challenge; it is a profound human-factors issue that can undermine the very adoption and effectiveness of AI, irrespective of its technical accuracy. Strategies to mitigate bias are crucial and include using diverse training datasets, implementing robust bias detection mechanisms, and ensuring continuous clinician oversight.
Clinician Trust, Acceptance, and Training
For AI to be successfully integrated, it must earn the trust of healthcare professionals. Clinicians may express skepticism or outright distrust in AI, particularly given the high-stakes nature of emergency medicine where mistakes can have severe consequences. The lack of transparency in how AI arrives at its decisions, often referred to as the "black box" problem, can further erode trust and make staff hesitant to fully embrace AI tools. There is also a concern that overreliance on AI could lead to a decline in emergency physicians' diagnostic and decision-making skills, potentially compromising patient care if an AI system provides erroneous responses that go unrecognized. Effective implementation therefore necessitates continuous staff training, clear explanations of AI's functionality and limitations, and fostering a data-driven culture where AI is perceived as a supportive partner rather than an inscrutable replacement. The success of AI is not solely determined by its algorithms or data, but by its integration into human workflows and its acceptance by human users. If clinicians distrust the AI or feel their skills are eroding, they will resist adoption or misuse the tools, rendering the technology ineffective.
Data Privacy, Security, and Accountability
AI-driven systems process vast quantities of sensitive patient information, making strict compliance with data protection regulations, such as HIPAA in the U.S. and GDPR in Europe, absolutely essential. The risks associated with data breaches, misuse, identity theft, and reputational damage are substantial. To counter these threats, robust security measures are paramount, including comprehensive data encryption (both at rest and in transit), secure storage solutions with stringent access controls (e.g., Role-Based Access Control (RBAC) and Multi-Factor Authentication (MFA)), and the implementation of granular, immutable audit trails for continuous monitoring. Techniques such as de-identification, pseudonymization, and the generation of synthetic data are vital for training AI models while safeguarding patient privacy. Furthermore, clear accountability frameworks are needed to define responsibilities when an AI system makes an incorrect decision, ensuring that ethical dilemmas are addressed and trust is maintained.
Regulatory Hurdles and Implementation Costs
Implementing AI solutions in healthcare is not a simple "plug-and-play" endeavor. It demands significant upfront investment in cloud infrastructure, data engineering expertise, AI specialists, and continuous model monitoring and retraining. Smaller clinics or public hospitals, in particular, may face substantial challenges in securing the necessary financial or human resources to support such initiatives. Regulatory scrutiny is exceptionally high for AI tools used in clinical decision-making, which can prolong the adoption timeline and introduce additional legal and administrative overhead. A further barrier to widespread adoption is the current lack of extensive supporting evidence from randomized controlled trials (RCTs), as most existing AI applications in this domain are based on retrospective studies.
The issue of poor data quality is not merely an inconvenience; it forms a critical upstream vulnerability that directly leads to algorithmic bias, which in turn can result in inequitable patient outcomes and even medical harm. The causal chain is clear: incomplete, inaccurate, or biased data leads to AI models trained on this flawed data, which then reinforces existing biases and inequalities. This results in inaccurate predictions or unfair treatment recommendations, ultimately causing under-triage, delayed care, resource misallocation, or even medical harm for specific patient groups. This cascade demonstrates that data quality is not just a technical prerequisite but a fundamental ethical and patient safety concern. Therefore, a primary strategic focus for EDs adopting AI must be on establishing rigorous data governance, cleansing, and standardization protocols before and during AI implementation. This proactive approach is essential to ensure AI serves as an equalizer rather than a perpetuator of healthcare disparities.
Real-World Impact: Case Studies in AI-Driven ED Optimization
The theoretical benefits of AI in emergency departments are increasingly being demonstrated through successful real-world implementations across various healthcare organizations. These case studies highlight the tangible improvements in patient flow, operational efficiency, and clinical outcomes.
Qventus
Qventus offers an AI-based SaaS solution that leverages AI, machine learning, and behavioral science to automate healthcare operations and significantly improve patient flow. Its impact has been notable across several key metrics:
Reduced Length of Stay (LoS): Qventus utilizes AI to facilitate early discharge planning by estimating discharge dates soon after admission. This has been shown to reduce extra hospital days by 15% to 30%, effectively freeing up beds and accelerating patient movement through the system.
Surgical Optimization: The solution has led to a reduction in surgery cancellations by up to 40% and an increase in the utilization of robotic surgeries by 36%.
Staff Productivity: Hospitals implementing Qventus have reported an increase in staff productivity by up to 50%.
Capacity Management: Qventus has assisted prominent hospitals like Boston Medical Center and HonorHealth in better managing their capacity and reducing the overall time patients spend in the hospital.
Financial Savings: Internally, Qventus achieved a 15% reduction in AWS cloud costs within the first six months, illustrating the cost-efficiency potential of AI solutions when applied to operational expenses.
Cleveland Clinic / Palantir Virtual Command Center
A strategic partnership between Cleveland Clinic and Palantir Technologies has resulted in the development of an AI-driven Virtual Command Center, designed for large-scale logistical coordination within the health system. This initiative has demonstrated significant impact through its modular components:
Hospital 360: This module provides a real-time display of patient census and forecasts capacity across Cleveland Clinic facilities. It enhances enterprise patient flow and resource planning, specifically improving bed management and patient transfers.
Staffing Matrix: This tool ensures that staffing levels are optimized based on predicted patient volume, offering more accurate forecasts than traditional models. This capability saves nurse managers considerable manual effort in shift planning.
OR Stewardship: Providing real-time insights into operating room scheduling opportunities and utilization patterns, this module assists with case-prediction analyses and Post-Anesthesia Care Unit (PACU) capacity estimates, thereby optimizing OR resources.
Discharge Streamlining: The system identifies outstanding tasks, such as imaging or consultations, to streamline the discharge process, which ultimately improves overall hospital efficiency.
Kaiser Permanente
Kaiser Permanente successfully implemented AI self-check-in kiosks in its clinics. The impact on patient experience and operational efficiency was substantial:
Approximately 75% of patients found these kiosks faster than interacting with clerks, and 90% were able to complete their check-in process without assistance. This significantly reduced front desk congestion, particularly during busy periods.
Yorkshire Ambulance Service (UK)
The Yorkshire Ambulance Service in the UK has deployed AI to enhance the efficiency of its call triage system.
The AI system analyzes real-time data, including the caller's description, tone of voice, and symptom keywords, alongside historical patterns to prioritize the most urgent cases. In trials, this system improved response times for critical conditions like cardiac arrest and stroke calls by flagging subtle signs that human operators might otherwise miss.
Other Notable Examples
One Medical Center (unnamed): This facility utilized AI predictive tools and implemented process changes that dramatically reduced the time for a patient to see a provider from 59 minutes to 14 minutes. Similarly, the time to get a room decreased from 37 minutes to 4 minutes, and the rate of patients leaving without being seen (LWBS) dropped from 5.3% to 2.4%.
Providence Health System: By integrating AI tools, Providence Health System successfully cut scheduling time from hours to just minutes.
Nahdi Pharmacy (Saudi Arabia): This pharmacy implemented an AI-powered WhatsApp queue management system, allowing patients to check in remotely and receive updates. This innovation effectively reduced lobby crowding and wait times.
Mayo Clinic: The Mayo Clinic has implemented AI-driven solutions to optimize revenue cycle management. Their AI models have demonstrated the ability to predict Emergency Department billing codes with over 92% accuracy for high-complexity cases.
While individual case studies demonstrate impressive metrics, the emphasis on phased rollouts and deliberate pilots underscores that successful large-scale AI integration is not a rapid deployment but an iterative process. This approach helps build trust and refines solutions over time. The initial cost and resource investment are justified by a long-term, incremental return on investment. The successful implementations by organizations like Kaiser Permanente, Qventus, and Cleveland Clinic illustrate that their achievements stem not just from possessing AI, but from how they strategically implemented it. Phased rollouts and deliberate pilots are crucial steps to mitigate risks such as data quality issues, algorithmic bias, and challenges in clinician trust. By starting small, validating the technology, and iteratively scaling, hospitals can refine models, address integration challenges, and build clinician buy-in, all of which are prerequisites for achieving the reported benefits and return on investment. Conversely, attempting a rapid, large-scale deployment without a well-conceived strategy can lead to significant failures, as seen in some instances like the UK's NHS Predictive Risk Stratification Model (PRISM).
The following table summarizes key performance indicators and outcomes from various AI implementations in emergency departments, providing a comparative overview of their impact.
Table 1: Key Performance Indicators (KPIs) and Outcomes from AI Implementations in Emergency Departments
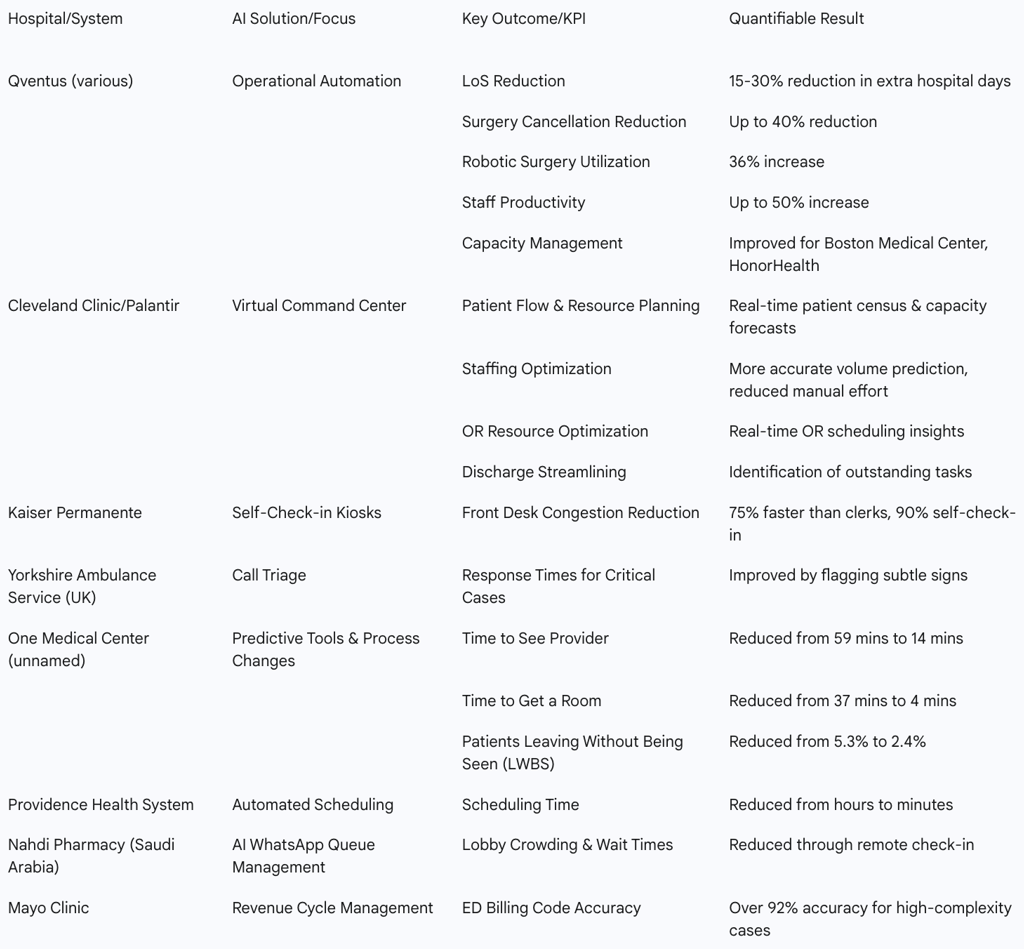
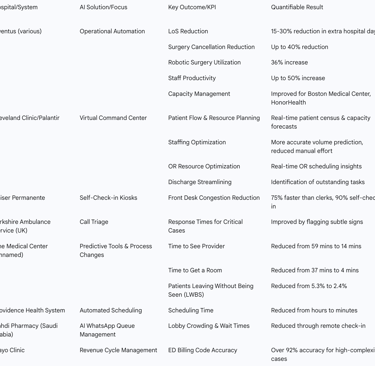
This table serves as a robust evidence base for healthcare executives and administrators. It allows for quick identification of relevant AI use cases that address specific pain points within their EDs. By providing concrete examples and quantitative data, it supports internal advocacy for AI adoption and informs strategic planning. The table implicitly suggests that a comprehensive AI strategy might involve combining several of these successful approaches to achieve multifaceted operational improvements and financial returns.
The Horizon of Emergency Medicine: Future Trends and Emerging Research
The trajectory of AI in emergency medicine points towards a future characterized by deeper integration, enhanced predictive capabilities, and a fundamental shift in how healthcare is delivered.
Integration with Wearable Health Technology and Remote Monitoring
A significant future trend involves the seamless integration of AI with wearable health technology. Devices such as smartwatches and portable ECG monitors are capable of continuously tracking patient vitals, feeding real-time health data directly into AI-driven systems. This continuous monitoring enables the early detection of deteriorating conditions, allowing for proactive intervention, particularly in high-risk patients, even before they present to the ED. Furthermore, AI-powered remote monitoring can extend care beyond hospital walls, supporting patients with chronic conditions or those recovering at home. This reduces reliance on periodic in-person check-ins and provides timely, data-driven signals to care teams, enhancing patient safety and peace of mind.
This integration signifies a fundamental shift in emergency medicine from a purely reactive model to one that increasingly incorporates proactive detection and even prevention. While current AI in EDs primarily optimizes the response to an emergency, continuous monitoring allows for the early detection of deteriorating conditions before they escalate into full-blown emergencies requiring an ED visit. This represents a strategic move up the healthcare value chain, from managing crises to preventing them or mitigating their severity at a much earlier stage. This is a shift from "emergency medicine" to "emergency prevention and early intervention."
The Role of Digital Twins in Simulating and Optimizing ED Environments
The concept of "Digital Twins"—virtual models of hospitals or specific departments like EDs—is gaining traction. These digital replicas can simulate patient flow, resource allocation, and various operational scenarios, allowing healthcare administrators to test interventions in a risk-free virtual environment before implementing them in real life. This technology enables precise experimentation with different operational strategies, optimizing resource allocation, and predicting outcomes with high fidelity. Leading companies like Siemens Healthineers are already utilizing AI-powered Digital Twin technology to predict patient health outcomes, paving the way for truly personalized medicine.
Advancements in Hyper-Personalized Care Pathways and Pre-Injury Prediction
AI's unparalleled ability to analyze vast amounts of data, including genetic information and social determinants of health, will enable the development of increasingly personalized care recommendations. This hyper-personalization can tailor treatment plans and care pathways based on an individual's unique physiological and psychological needs, moving beyond generalized protocols. An even more ambitious area of emerging research proposes that AI technologies could predict the time of injury occurrence. By analyzing factors such as weather conditions, vehicle features, time of day, and historical accident data, AI aims to enable pre-emptive measures to prevent injuries before they happen.
The Vision of AI-Powered Digital Hospitals and Networked Emergency Departments
The future envisions an "AI-powered digital hospital" where continuous data collection and processing provide real-time estimates of bed availability and optimize patient movement across departments. This concept extends to networked emergency departments within a region or state, establishing a system for improved real-time visibility of bed availability and specialized care capacity across multiple facilities. Such networked intelligence can lead to more efficient resource allocation and dynamic adaptation to emergency situations on a broader, systemic scale. Furthermore, AI will seamlessly integrate with Electronic Health Records (EHRs) to automate patient outreach, offer real-time scheduling adjustments (e.g., prioritizing urgent cases), and personalize communications, all without overburdening staff.
The vision of AI-powered digital hospitals and networked EDs suggests that AI's true transformative power will be realized not just within individual departments, but through the seamless integration and intelligence sharing across an entire healthcare ecosystem. Current challenges often stem from fragmented data and communication breakdowns between teams. A "networked ED" or "digital hospital" model, powered by AI, directly addresses this by creating a unified, real-time data environment. This allows for dynamic load balancing, optimal patient placement across facilities, and proactive resource allocation beyond a single ED. It is about optimizing the entire patient journey across different care settings.
Other Key Advancements and Emerging Research
Beyond these core trends, several other advancements are shaping the future of emergency medicine:
Ambient Listening: Solutions like Nuance DAX are revolutionizing documentation by converting doctor-patient conversations into structured clinical notes in real-time, significantly reducing the administrative burden on clinicians.
Smarter Imaging: AI models are being trained to identify subtle signs of disease in medical images (e.g., lung scans, mammograms, external eye photos) that human eyes might miss, leading to earlier and more accurate diagnoses.
Phenomics: AI will efficiently process and analyze high-dimensional phenotypic data (e.g., gene expression, proteomics, metabolomics, medical imaging) to discover hidden patterns and associations. This will provide deeper insights into disease mechanisms and drive precision medicine.
Surgical Automation: AI is expected to advance surgical robots, improving precision and efficiency in complex surgical procedures.
Drug Discovery: AI is accelerating the identification of new drug candidates and optimizing drug design processes, significantly reducing the time and cost associated with bringing new therapies to market.
Strategic Recommendations for AI Adoption in Emergency Departments
For healthcare organizations aiming to leverage AI and predictive analytics for optimized ED flow, a strategic and deliberate approach is essential.
A Phased Approach to Implementation, Emphasizing Pilot Programs and Continuous Evaluation
Successful AI adoption begins with a clear, well-defined use case that directly addresses specific business needs and objectives within the ED. It is recommended to initiate with pilot programs to test AI solutions in real-world settings. These pilots allow for assessment of effectiveness, identification of areas for refinement, and building internal confidence before broader deployment. An iterative scaling approach should be adopted, where learnings from early implementations continuously inform and improve the models and integration processes. Prioritizing solutions that demonstrate resilience to data shifts and incorporate Machine Learning Operations (MLOps) architecture for continuous updates is crucial to maintaining accuracy and efficiency over time. This approach recognizes that the initial investment in AI should be viewed as a foundational commitment to a long-term digital transformation, not a quick fix.
Prioritizing Robust Data Governance and Infrastructure Development
Investment in robust technical infrastructure is non-negotiable. This includes adequate hardware, computing power, and strong IT systems capable of handling the large volumes of real-time data required by complex AI algorithms. Simultaneously, establishing comprehensive data governance policies is paramount, focusing on data quality, completeness, and standardization across disparate sources such as EHRs, laboratory systems, and wearable devices. Implementing rigorous data minimization strategies, collecting and processing only the absolute minimum necessary patient health information (PHI), is also vital for privacy and security. Finally, ensuring seamless integration with existing health IT systems (e.g., EHRs, PACS) is critical to avoid disrupting established workflows and to maximize the utility of available data.
Developing Comprehensive Ethical Frameworks and Bias Mitigation Strategies
Proactive measures to address algorithmic bias are essential. This involves using diverse training datasets, implementing sophisticated bias detection mechanisms, and regularly auditing predictive models for fairness and accuracy across all patient populations, especially vulnerable groups. Establishing clear ethical guidelines and accountability frameworks for AI decision-making is necessary, explicitly defining responsibilities in cases of error. Prioritizing transparency in AI models through explainable AI techniques is crucial to building clinician trust and allowing for informed human oversight and the ability to challenge AI recommendations. Furthermore, strict compliance with data privacy regulations (e.g., HIPAA, GDPR) must be ensured through robust encryption, access controls, and de-identification techniques. Obtaining informed patient consent for data collection and AI involvement in their care, along with providing clear explanations of data usage, is also a fundamental ethical requirement.
Investing in Clinician Education, Training, and Fostering Interdisciplinary Collaboration
The successful adoption of AI in EDs hinges fundamentally on human factors: trust, education, and collaboration. It is imperative to provide continuous training and education for all staff—clinicians, IT personnel, and administrators—on how AI systems function, their benefits, limitations, and the associated ethical considerations. Fostering clinician acceptance is achieved by involving them early in the planning and pilot phases, highlighting use cases where AI directly improves patient outcomes and reduces administrative burden. It is crucial to emphasize AI as an augmentation tool that supports human expertise, rather than a replacement, to mitigate fears of job displacement or skill erosion. Finally, promoting interdisciplinary collaboration among physicians, data scientists, IT specialists, and policymakers is essential for effectively developing, implementing, and refining AI solutions. The investment in AI should be equally weighted between technological infrastructure and human capital development, including fostering critical thinking skills in an AI-augmented environment and creating platforms for continuous feedback between clinicians and AI developers.
Conclusion
AI and predictive analytics are no longer theoretical concepts but have emerged as practical, transformative forces poised to revolutionize emergency medicine. They offer a compelling pathway to address the critical and persistent challenges faced by Emergency Departments, including overcrowding, prolonged wait times, and resource constraints. The evidence strongly supports AI's capacity to deliver measurable benefits across operational, clinical, and financial dimensions, from significantly reducing wait times and improving diagnostic accuracy to optimizing resource allocation and realizing substantial cost savings.
The current state of EDs, often described as chaotic and prone to overcrowding, reflects systemic and growing challenges. AI's ability to optimize patient flow, manage capacity, and automate tasks directly addresses the core operational fragility of emergency care. Without these efficiencies, the system is increasingly unsustainable under rising demand and existing workforce shortages. This means AI is becoming essential for the long-term sustainability and resilience of emergency care systems; without it, EDs risk being overwhelmed, potentially leading to systemic failures. Therefore, AI is not merely an improvement tool but is rapidly becoming a necessity for maintaining the viability of emergency care, not just enhancing it.
Successful integration of AI requires a deliberate, strategic approach that prioritizes robust data quality, comprehensive ethical considerations, proactive clinician engagement, and a commitment to continuous learning and adaptation. As healthcare demands continue to grow and evolve, AI represents an indispensable tool. It supports clinicians, enhances the delivery of high-quality care, and prepares EDs for the complex challenges of modern medicine. The future of emergency medicine will be characterized by interconnected, intelligent, and increasingly automated systems that empower healthcare providers to deliver faster, more precise, and ultimately, life-saving care, ensuring the ED can continue to fulfill its critical role effectively in the face of escalating pressures.
FAQ Section
What is AI triage in emergency departments? AI triage in emergency departments refers to using artificial intelligence algorithms to analyse patient data and determine the urgency and appropriate level of care needed. These systems typically use machine learning to process multiple variables, including vital signs, symptoms, medical history, and demographic information, to predict patient acuity more accurately than traditional triage methods.
How does predictive analytics improve emergency department flow? Predictive analytics improves ED flow by forecasting patient volume, resource needs, and likely bottlenecks before they occur. These systems analyse historical data patterns to anticipate hourly, daily, and seasonal demand fluctuations, allowing hospitals to optimise staffing, bed management, and resource allocation proactively rather than reactively.
What percentage improvement in wait times can hospitals expect from implementing AI triage? Hospitals implementing AI triage systems typically report average wait time reductions of 20-30%, with some institutions achieving improvements of up to 40-60% during peak periods. The exact improvement depends on factors including baseline efficiency, implementation approach, and how comprehensively the AI system is integrated with existing workflows.
Does AI triage replace human clinicians in the emergency department? AI triage does not replace human clinicians but augments their capabilities. These systems serve as decision-support tools that help identify high-risk patients and optimize resource allocation while healthcare professionals maintain final clinical judgment and provide the human elements of care, including empathy and complex decision-making.
What data is required to implement predictive analytics in an emergency department? Implementing predictive analytics typically requires historical ED visit data (at least 1-2 years), including arrival times, patient demographics, acuity levels, chief complaints, length of stay, disposition, and resource utilisation. Additional valuable data includes staffing patterns, local event calendars, weather data, and regional healthcare utilisation trends.
How long does it typically take to implement AI triage and predictive analytics systems? Full implementation typically takes 9-24 months, with the timeline varying based on organisational readiness, data availability, and implementation scope. Most successful deployments follow a phased approach, with limited pilots demonstrating value before expanding to comprehensive integration across all emergency department functions.
What are the main ethical concerns related to AI triage in emergency care? The main ethical concerns include algorithmic bias that may disadvantage certain demographic groups, privacy considerations related to sensitive patient data, questions about transparency and explainability of AI decision-making, and responsibility/liability issues when algorithms influence clinical decisions. Ongoing monitoring and governance are essential to address these concerns.
How do AI triage systems handle patients with complex or unusual presentations? Advanced AI triage systems are designed to flag unusual or complex presentations that don't fit standard patterns, ensuring these cases receive appropriate clinical attention. Many systems incorporate confidence scores with their predictions and are programmed to recommend higher levels of care when uncertainty exists, minimising the risk of undertriage for atypical cases.
What ROI can hospitals expect from implementing AI-enhanced ED flow optimisation? Hospitals typically report ROI ranging from 200-400% within 2-3 years of implementation, with financial benefits stemming from reduced labour costs through optimised staffing, decreased left-without-being-seen rates, improved billing capture, and reduced liability exposure. Additional value comes from improved patient satisfaction scores and quality metrics.
How does AI triage impact emergency department staffing requirements? AI triage doesn't necessarily reduce overall staffing requirements but helps optimise when and where staff are deployed. Predictive systems allow for more precise staffing alignment with anticipated demand patterns, potentially reducing overtime costs while improving care quality through more appropriate distribution of clinical resources when and where they're most needed.
Additional Resources
For readers interested in exploring AI triage and predictive analytics in emergency departments further, the following resources provide valuable insights:
The AI-Powered Hospital: How Artificial Intelligence is Transforming Medicine by Dr. Eric Topol (2023) - A comprehensive examination of AI applications in healthcare, with detailed chapters on emergency medicine applications and implementation strategies.
Journal of the American Medical Informatics Association Special Issue on AI in Emergency Care (2024) - A collection of peer-reviewed research articles detailing the latest advances in AI applications for emergency medicine, including multicenter studies on implementation outcomes.
Emergency Department Optimization Toolkit by the Institute for Healthcare Improvement—This is a practical guide for healthcare leaders implementing process improvements in emergency settings. Recent additions cover AI integration and change management strategies.
"Implementing AI in Emergency Medicine: Ethical Framework and Best Practices" - A consensus statement from the American College of Emergency Physicians guiding responsible AI implementation with particular attention to bias mitigation and governance structures.
HealthTech Magazine's "Predictive Analytics in Healthcare" Resource Hub - A regularly updated collection of case studies, implementation guides, and technology reviews focused on predictive analytics applications in various healthcare settings, including emergency departments.
